Current state and future perspectives of sleep medicine and sleep research in Armenia
A Joint Position Statement of Armenian Sleep Disorders Association, Armenian National Institute of Health, and European Assembly of National Sleep Societies
Khachatryan S.G.,1,2,3, Isayan M.A.,1,2 Hovakimyan H.A.,1,2 Deleanu O.,3,4,5 Korostovtseva L.,3,6 Verbraecken J.,3,7 Van der Werf Y.D.,3,8 Bazarchyan A.A.,9 Gnidovec-Stražišar B.3,10
1Armenian Sleep Disorders Association, Yerevan, Armenia
2Department of Neurology and Neurosurgery, National Institute of Health, Yerevan, Armenia
3Executive Committee, Assembly of National Sleep Societies of European Sleep Research Society
4University of Medicine and Pharmacy Carol Davila, Bucharest, Romania
5Institute of Pneumophtisiology M. Nasta, Bucharest, Romania
6Almazov National Medical Research Centre, St Petersburg, Russia
7Multidisciplinary Sleep Disorders Centre, Antwerp University Hospital and University of Antwerp, Antwerp, Belgium
8Department of Anatomy and Neurosciences, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam Neuroscience, Amsterdam, The Netherlands
9National Institute of Health, Yerevan, Armenia
10Paediatric Department, General Hospital Celje, Celje, Slovenia
ABSTRACT
This article represents a brief overview and summary of the main ideas, suggestions, agreements, and conclusions reached during a special round-table discussion held on Oct 10, 2019, at the Armenian National Institute of Health, with the participation of representatives from the Armenian Sleep Disorders Association and the Executive Committee of the Assembly of National Sleep Societies (ANSS) of the European Sleep Research Society. As the pilot activity of the ANSS “Beyond Boundaries” project, it aimed to identify the current needs in the field of sleep medicine in Armenia and to summarize the recommendations to help improving the future multidisciplinary development of this important field in Armenia. The article aims to serve as a guiding point for further collaborations regarding sleep medicine in Armenia. Based on the evaluation of this pilot project, the ANSS will further shape and improve the “Beyond Boundaries” project for further implementation in other European countries that wish to develop knowledge and skills in the field of sleep medicine and research and broaden their international network.
Keywords: Armenia, sleep, sleep medicine, sleep research, position statement, ANSS, ESRS, ARSDA
DOI:10.54235/27382737-2021.1.1-28.
ROUND-TABLE PARTICIPANTS
ARSDA Samson Khachatryan (also ANSS), Haykuhi Hovakimyan, Mariam Isayan.
ANSS Executive Board members Barbara Gnidovec-Stražišar (President), Lyudmila Korostovtseva (Secretary), Ysbrand van der Werf (Treasurer), Oana Deleanu, Johan Verbraecken.
ANIH Alexander Bazarchyan (Director), Diana Andreasyan (Head of Health Information and Analysis Center), Gohar Yerimyan (Dean of Medical Faculty).
Representatives of other Armenian governmental and non-governmental organizations.
INTRODUCTION
Sleep-related complaints and sleep disorders are common in general population [1-4]. Sleep disorders can cause various primary and secondary problems that need to be identified, diagnosed, and treated. Sleep research and sleep medicine both are established fields in the European Union (EU) and the United States (US). But in many countries, especially in the developing countries, sleep as an essential part of the health and health care system is not represented properly. In Armenia sleep research and sleep medicine is a rather new and developing field and has already engendered numerous activities such as seminars, congresses, short trainings, conferences, surveys, and clinical research studies. Still, many issues remain unsolved and there are serious obstacles hampering the implementation of clinical and fundamental knowledge. In October 2019, a round-table organized by the Armenian Sleep Disorders Association (ARSDA), the Assembly of National Sleep Societies (ANSS) of the European Sleep Research Society (ESRS), and the Armenian National Institute of Health (ANIH) was carried out in Yerevan, Armenia. As a very important activity for the development of sleep medicine in Armenia, the results and recommendations of this meeting are summarized in the following text for future reference.
SLEEP AND ITS DISORDERS
Sleep is a vital physiological function of the human organism. It is an active and multicomponent process. As can be seen using polysomnography (PSG), in normal conditions the human sleep consists of two main types: rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. NREM sleep itself is subdivided into various stages of depth. The REM and NREM sleep stages alternate throughout the night in normal sleep. Good quality sleep plays an essential role in our physical, mental and emotional health and development, while poor sleep and sleep deprivation negatively affect physiological and mental processes. These negative effects become increasingly evident when sleep problems become chronic.
There are 3 systems for the classification of sleep disorders: International Classification of Sleep Disorders 3rd Edition (ICSD-3) [5], International Classification of Diseases, 10th Revision (ICD-10) [6], and Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) [7]. The ICSD-3 distinguishes six main groups of sleep disorders:
► Insomnias
► Sleep-related breathing disorders
► Central disorders of hypersomnolence
► Circadian rhythm sleep-wake disorders
► Parasomnias
► Sleep-related movement disorders
SLEEP DISORDERS AND MEDICAL COMORBIDITIES
As sleep constitutes an intricate physiological state, it is not surprising that sleep has complex relationships with other mental and somatic disorders. Comorbidities are very common and their impact on patients’ overall condition often influences the course of the disorders. The relationship of sleep disorders and comorbid medical conditions are bidirectional and treatment of sleep disorders or sleep disturbance can improve the comorbid condition and vice versa. For instance, a study from Armenia suggests that restless legs syndrome (RLS) is significantly more common among patients with epilepsy (20.6%) than in healthy individuals (8%) [8].
Sleep problems are common in neurological disorders. Insomnia and obstructive sleep apnea (OSA) are the most frequent sleep disorders among patients with epilepsy and headache. Circadian rhythm sleep disturbance can occur in the early stage of Alzheimer’s disease and can worsen as the disease progresses. OSA is also a frequent condition in Alzheimer’s disease [9,10].
In Parkinson’s disease, insomnia, REM-sleep behavior disorder (RBD), sleep-disordered breathing (SDB) and RLS are the most common sleep disorders. Almost 80% of patients with Parkinson’s disease have sleep fragmentation and early morning awakenings [11]. In Armenian Parkinson’s disease patients, the comorbidity with RLS was also very frequent (39%), especially among females [12].
Sleep disorders are highly comorbid with chronic pain and diabetes, as well as with various other neurological disorders like stroke and multiple sclerosis, cardiovascular, respiratory, gastrointestinal, urinary disorders, iron deficiency, kidney disease, diabetes, autoimmune disorders and others [13-16].
Sleep complaints and sleep disorders are highly prevalent in psychiatric disorders, especially in major depressive disorder, generalized anxiety disorder, bipolar disorders, post-traumatic stress disorder, schizophrenia, substance abuse, and others [17,18].
SLEEP DISORDERS AND MORTALITY
Sleep disorders are associated with an increased mortality risk. In a review article employing meta-analysis, the authors concluded that sleeping more (9-10 h) than the recommended 7-9 hours was associated with a 33% risk of all-cause mortality [19,20]. Longer sleep can be associated with mortality compared to healthy people who have no serious mental and somatic health problems [21]. On the other hand, fragmented and short sleep, for example in the case of OSA, can also be a serious risk factor for mortality [22,23]. A study by the Armenian group that looked into the prevalence of road accidents caused by sleep disorders showed that insomnia was more common in people who had road accidents (69.0%, p < 0.05). Also sleep apnea was mostly seen in people with road accidents (41.4% vs 19.5%, p < 0.01) [24].
SLEEP DISORDERS AND SUICIDE RISK
Some types of sleep disorders, such as insomnia and nightmares, can be risk factors for suicidal ideations and suicidal behavior among patients with depression [25]. There are, however, findings that suicidal ideation and behaviors can also occur among patients with sleep complaints and sleep disorders without depression, which might be connected to serotonergic transmission [26].
ECONOMIC BURDEN OF SLEEP DISORDERS
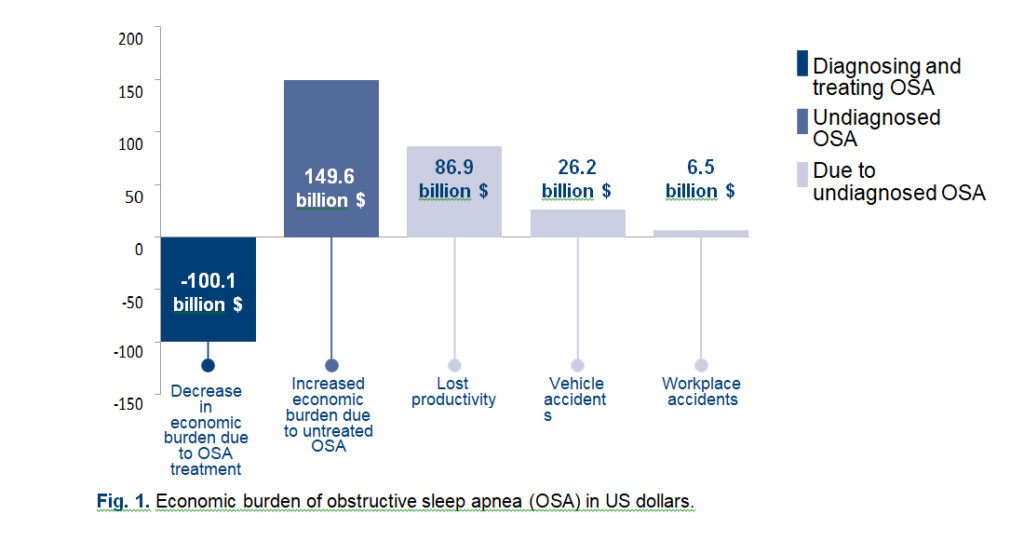
Sleep disorders can cause economic issues if they remain undiagnosed and untreated. Several studies show the extent of economic loss for individuals and the country as a whole [27,28]. For example, in the US diagnosing and treating all cases of OSA would decrease the economic burden up to $100.1 billion annually. Conversely, undiagnosed OSA increases the economic burden by approximately $149.6 billion in the US annually. This cost includes $86.9 billion in lost productivity, $26.2 billion in motor vehicle accidents, and $6.5 billion in workplace accidents (Fig.1).
Untreated OSA is also a risk factor for diseases requiring high-value treatment, and is associated with hypertension, heart disease, diabetes, and depression. This sums up to approximately $30 billion for health care utilization and medication for these comorbid health risks [28].
SLEEP DISORDERS AND QUALITY OF LIFE
As evidenced from the above, sleep disorders are strongly associated with patients’ quality of life (QOL) through problems with mental and somatic health, while at the same time being a reason for noticeable economic burden. Disordered sleep decreases QOL and various studies show that treatment of sleep disorders can improve health-related quality of life [29,30].
JOINING FORCES TOWARDS THE IMPROVEMENT OF SLEEP MEDICINE IN ARMENIAINING FORCES TOWARDS THE IMPROVEMENT OF SLEEP MEDICINE IN ARMENI
The above-mentioned domains are the most noticeable (prevalence, comorbidity, QOL, economic burden) and alarming topics (mortality, suicidal risk) that are connected to sleep and its disorders. These are essential parts of daily life and healthcare, economic, epidemiological, educational systems in all countries. A systematic approach is therefore needed to overcome the present situation. Healthcare providers, educational structures, governmental institutions, insurance companies, NGOs, and many other organizations that are involved in healthcare also in Armenia are not aware of the sleep medicine field and of these serious health outcomes that occur due to the underrecognition of sleep disorders.
The ESRS is the main organization in Europe incorporating the best clinical and scientific aspects of sleep medicine and sleep research activities. It promotes sleep research, improvement of care among patients with sleep disorders, facilitates the dissemination of knowledge regarding sleep medicine and sleep research through scientific meetings, educational seminars and researcher training awards [31]. The ANSS is an organization that brings together European national sleep societies with the common goal to develop sleep medicine and sleep research in Europe. The ANSS is a formal body of the ESRS and represents the associate members from different European countries. The ESRS admits national sleep societies as associates to the ANSS. The ANSS is governed by the ANSS EC [32]. Thirty-one European national sleep societies and a total of over 7500 associate members are involved in the ANSS. ARSDA is a non-governmental organization representing and promoting sleep medicine and sleep research in Armenia. ARSDA is a member of the ESRS-ANSS since 2012. ARSDA was founded in 2011 by Samson Khachatryan – the current pre-
sident of the Association.
The ANIH is an organization within the system of the Armenian ministry of Health (MOH). The ANIH is focused on gathering health statistics and preparing professionals in the medical field, developing and implementing different approaches for a better functioning healthcare system. The current director of the ANIH is Dr. Alexander Bazarchyan.
For the above-mentioned purpose, a series of joint meetings was conducted on October 10-11, 2019, in Yerevan, Armenia. Executives of the ARSDA, ANSS, and ANIH gathered to discuss current problems and stimulate the creation of future opportunities to develop sleep medicine in Armenia, introducing their own experience, methods, and sleep medicine programs.
ARMENIAN SLEEP DISORDERS ASSOCIATION
ARSDA is a non-governmental organization (NGO) founded in 2011. It is the only organization in Armenia that addresses its activities towards the development and dissemination of sleep medicine and sleep research. ARSDA aims to develop the field of sleep medicine in Armenia and thereby filling an important gap in Armenian medicine. The mission of ARSDA is to promote sleep health, education in sleep medicine and its development as a field, and interest in sleep research in Armenia. On the way to reach its goals, ARSDA has organized numerous events, partly within the framework of the World Sleep Day celebrated annually by the World Sleep Society. Through the years, ARSDA has collaborated with other organizations by including sleep topics in the programs of their narrow-field congresses and seminars. A very important part is collaborating with medical and psychology students. ARSDA has established important relations with different institutions like the ANIH, Yerevan State Medical University (YSMU), and its young researchers’ structures and Yerevan State University’s Faculty of Philosophy and Psychology. ARSDA is a member of the ANSS-ESRS supported by other professional societies and has organized a multitude of seminars, meetings and round-table discussions. Taking into consideration the importance of having local epidemiological data on sleep disorders, ARSDA organized a survey on the prevalence of sleep-related complaints and disorders in different regions of Armenia during recent years. With the help of this project, ARSDA now possesses important information on the prevalence of different sleep disorders among the general adult population of Armenia that will aid and inform future activities [33]. For many years, ARSDA members have collected pertinent knowledge of the situation with sleep medicine and have witnessed a slow but steady growth of awareness, especially among physicians and the general public in Yerevan. Sleep disorders remain a serious problem for Armenia, however, especially for particular regions.
Table 1. Prevalence of sleep disorders and sleep-related complaints in Armenian population
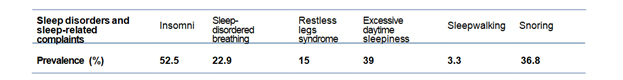
The main problems that sleep medicine development faces in Armenia are a lack of awareness of sleep disorders among physicians, an absence of governmental coverage for diagnostic studies and treatments, lack of newer drugs, problems with importing the devices, ignorance of “sleepiness at the wheel” issue, and others (Table 1). To address these issues, on October 10-11, 2019 ARSDA hosted the ANSS-EC meeting, a round-table discussion and a full day educational seminar on sleep disorders. Current problems in sleep medicine in Armenia were discussed during this meeting involving public health authorities. The meeting addressed issues essential for raising awareness of the importance of sleep professional skills and knowledge, and identified crucial points interfering with the development of sleep medicine that will be discussed in this paper.
PREVALENCE OF SLEEP DISORDERS IN ARMENIA AND OTHER COUNTRIES
The study of sleep disorders is becoming increasingly popular nowadays as these problems are frequently encountered and carry serious public health implications. According to the American Sleep Association, approximately 50-70 million Americans have sleep problems and sleep disorders, in particular, 48.0% snoring, 37.9% sleeping during the day, and 4.7% sleeping while driving. Thirty percent have short-term insomnia and 10% have chronic insomnia. Obstructive sleep apnea is also common, especially among men – 24-31% [34]. In Eastern Europe, insomnia (20%) was among the most common mental health problems, along with depression, anxiety, and alcohol misuse according to an internet survey implemented by Voinescu et al. [35]. Sleep problems are present not only among adults, but also among children and adolescents [36,37]. Disorders of sleep are similarly common in Armenia as the results of a multi-site door-to-door study suggest [33].
A door-to-door survey was conducted in Armenia and aimed to investigate sleep-wake patterns, sleep-related habits, and the prevalence of sleep disorders among the Armenian population, includ- ing insomnia, excessive daytime sleepiness (EDS), SDB (e.g. snoring, OSA), RLS, etc. The survey was conducted in 4 different regions of Armenia: Akner (Syunik region), Bagratashen (Tavush region), Ayrk/Verin Shorzha (Gegharkunik region) villages, and Yerevan city (the capital of Armenia). Overall 1001 participants aged 18 years and older (mean age 45 years, females – 67.5%) were interviewed. The questionnaire consisted of 27 questions, most of them with yes/no answers. The results from this survey spread light on the prevalence of sleep dis- orders among the Armenian population, as this was the first of its kind large research project in this field. As the results show, the most frequent sleep disorders were insomnia and SDB (see Table 1).
DIAGNOSTICS AND TREATMENT OF SLEEP DISORDERS IN ARMENIA
EDS is objectively assessed through special poly- somnographic protocols. The maintenance of wake- fulness test (MWT) is a sensitive sleep detection test that assesses the ability to stay awake, and is used for identification of possible sleep episodes that might escape the patient’s attention. MWT is commonly used among truck drivers. It is known that driving for long distances may lead to EDS, whereas SDB might be a contributing factor for accidental sleep and, therefore lead to traffic near-misses as well as vehicle crashes. The multiple sleep latency test (MSLT) is another protocol commonly used in sleep medicine practice. The MSLT protocol tests the abil- ity of an individual to fall asleep during the daytime while being in a sleep-predisposing environment. This method is used for the diagnosis of hypersom- nolence disorders, particularly for the diagnosis of narcolepsy, but it is also considered a useful tool to test excessive daytime sleepiness (EDS) in drivers. Unfortunately, these tests are not widely available in Armenia. Moreover, those are mostly not reim- bursed by state and private insurance organizations. Currently, pharmacological and non-pharmaco- logical approaches are used to treat insomnia. In both European and American guidelines, cognitive behavioral therapy for insomnia (CBT-I) is the preferred choice of treatment for chronic insomnia. There are difficulties, however, with the evidence-based man- agement of acute insomnia, since there are no clear instructions on this problem in the guidelines. In Armenia, the treatment of insomnia is more compli- cated, since the patients usually come to physicians only late after the onset of insomnia. Difficulties with implementing treatment for insomnia arise also be- cause CBT-I is not always available due to generally poor understanding of psychotherapy, financial diffi- culties, lack of qualified specialists, etc.
The management of SDB firstly requires diag- nostic workup through PSG or polygraphy (PG). The severity of OSA, as well as other kinds of SDB requires special approaches in treatment. Continuous Positive Airway Pressure (CPAP), Bilevel Positive Airway Pressure (BPAP), and Non-Invasive Ventilation (NIV) are non-pharmacological means of treatment for OSA. In many European countries, apnea screening, as well as PAP treatment, are re- imbursed by either government or by insurance companies. However, in Armenia OSA is underdi- agnosed because of a low level of apnea detection among local medical professionals, and due to high costs and absence of reimbursement. Other modali- ties of SDB treatment, including oral appliances and obesity control, are not represented enough or well integrated within the scope of SDB management.
THE ANSS “BEYOND BOUNDARIES” INITIATIVE AND ITS PILOT PROJECT IN ARMENIA
As a body incorporating sleep societies from different European countries, the ANSS faces a situation of varying levels of sleep medicine devel- opment across the European territory. There are serious differences between countries, their health systems, and coverage of sleep disorders. The issue of promoting sleep medicine in countries with low or middle levels of sleep medicine was voiced more strongly after representatives of Eastern European countries were elected to the ANSS EC. During ex- ecutive committee meetings of the ANSS this top- ic has been proposed and discussed in detail. It subsequently developed into an initiative for sleep medicine development in such countries.
The ANSS executive committee created the “Beyond Boundaries” project for the European countries that are interested in assistance for sleep medicine development. The project included shar- ing experience gained by developed countries, promoting good sleep habits in the general population, striving against stigmas, advocating for health au- thorities and related organizations, and implement- ing financial support mechanisms for patients with sleep disorders, etc. It was approved by the ANSS member societies, as well as by the ESRS board further gaining official support from the ESRS.
It was proposed to hold the pilot event for the “Beyond Boundaries” project in Armenia. Within the main project held in Armenia it was decided to organize a meeting for different governmental and non-governmental organizations which could help promote and develop sleep medicine in Armenia, accentuate its public health role and stimulate a re- alistic and useful discussion between the involved sides.
GENERAL DESCRIPTION OF THE EVENT AND PARTICIPANTS
The ARSDA, ANSS EC, and ANIH joint meeting was organized on October 10th, 2019, in Yerevan, Armenia. The meeting was held in a form of a round-table discussion at the ANIH headquarters involving participants from various sleep medi- cine-related health fields.
The ANSS EC was represented by the President
- Barbara Gnidovec-Stražišar, Slovenia (pediatric neurologist), Oana Deleanu, Romania (pulmonolo- gist), ANSS EC secretary Lyudmila Korostovtseva, Russia, (cardiologist), Johan Verbraecken, Belgium, (pulmonologist), Samson Khachatryan, Armenia, (neurologist), and ANSS treasurer Ysbrand van der Werf, The Netherlands (sleep neuroscientist). Samson Khachatryan also represented the ARSDA in his role as president together with other Dr. Alexander Bazarchyan was leading the ANIH group as the director of ANIH and was the host of the meeting. Representatives of various departments of the ANIH additionally contributed. Dr. Narek Baghdasaryan – a clinical pharmacologist who rep- resented the Scientific Center of Drug and Medical Technologies Expertise (SCDMTE, the national drug regulation agency) and shared important ideas on the sleep drugs which are currently not available.
For the round table discussion, representa- tives of the Ministry of Finances, the Ministry of Transport and Communication, Police, chairs of Public Health departments from the YSMU and the American University of Armenia, representatives of insurance companies, and other related non-gov- ernmental bodies were invited. There was a not- ed absence of these parties at the event, however, which likely indicates the low level of their appreci- ation of the problem.
ROUND TABLE DISCUSSION
The session was chaired by Drs. Alexander Bazarchyan, Samson Khachatryan, and Barbara Gnidovec-Stražišar. The session chairs presented their opening speeches and then proceeded with the respective presentations and discussions.
DR. BARBARA GNIDOVEC-STRAŽIŠAR ABOUT ANSS “BEYOND BOUNDARIES” PILOT PROJECT
Dr. Gnidovec-Stražišar presented the ANSS past activities such as work on European guide- lines for accreditation of Sleep Medicine Centers, certification of professionals in sleep medicine, standard procedures for adults in accredited sleep medicine centers in Europe, the catalogue of knowledge and skills for sleep medicine. Dr. Gnidovec-Stražišar subsequently introduced the ANSS aims, such as admitting sleep medicine as a subspecialization, accreditation of sleep centers and sleep professionals, professional education is- sues in sleep medicine, reimbursement for sleep diagnostics and treatment.
Currently, the ANSS works on helping the devel- opment of sleep medicine and sleep research fields in Europe (including countries beyond the EU) by expanding and harmonizing the level of knowledge among sleep professionals via guidelines and oth- er projects including teaching courses for sleep professionals. The “Beyond Boundaries” project was developed by the ANSS to spread knowledge on sleep medicine in countries that are interested in assistance in sleep medicine development. The program is set up to adapt to the needs of a partic- ular applicant country. The main issues the ANSS may educate are setting up a sleep lab in a country with low financial income and lack of reimburse- ment, lobbying for reimbursement, developing and running educational programs, organizing national sleep conferences and courses, starting to develop sleep medicine in a country with low income, and seeking for sources of financial support.
A different aspect of the ANSS workload is to help national sleep societies to develop a network of accredited sleep centers. The first steps are to identify the needs of countries seeking to increase local clinical and scientific education, recognize the specific needs in training and create an individual- ized program for each country, create a network of local experts to assist and support them by in- creasing local potential for formal education by the means of tailored workshops. The ANSS can support sleep medicine development by organizing special meetings with health and other authorities and related organizations to expand education and collaboration for sleep medicine professionals.
DR. SAMSON KHACHATRYAN ABOUT PREVALENCE OF SLEEP DISORDERS IN ARMENIA
The next topic was presented by the ARSDA president and the ANSS EC member Samson Khachatryan presenting the development of sleep medicine and epidemiology of sleep disorders in the Armenian population. He presented ARSDA epidemiological study results, which were ac- quired during a large cross-sectional door-to-door anonymous survey study. It was conducted at four different sites of Armenia and data of 1001 adult participants was gathered from the general pop- ulation. As the study showed, insomnia, EDS, and SDB are among the most prevalent issues within the Armenian adult population. Movement disor- ders of sleep, such as RLS, had a high incidence with varying distribution depending on the altitude. Insomnia was present in about half of the partici- pants. Snoring and witnessed apnea were present in around the third of the studied population.
Dr. Samson Khachatryan shared experience of different teaching events, meetings, confer- ences ever organized in the sleep medicine field in Armenia including WSD activities, and presented current issues accumulated in the field, and sum- marized future perspectives of developing sleep medicine in Armenia.
DR. OANA DELEANU ABOUT SLEEP MEDICINE DEVELOPMENT EXPERIENCE IN ROMANIA
The ANSS EC member pulmonologist Oana Deleanu delivered an important presentation en- titled the “Role of sleep and its disorders for pub- lic health – Romanian Experience”. In her speech she tried first to answer some important questions, such as what is sleep, why is it important, what kind of sleep disorders are present, economic costs of short sleep duration, insomnia, OSA, and after this she shared the Romanian experience.
Oana Deleanu mentioned that an important part of sleep medicine development is to have educated and motivated physicians – both clinical and re- search specialists involved in sleep. To motivate and interest them requires the organization of cours- es, to invite visiting professors, apply for bursaries and fellowships, pass the ESRS sleep expert exam- ination and promote networking among European academic and sleep centers. Also, opening sleep facilities and approving sleep medicine as a spe- cialization or subspecialization, giving a master’s degree in sleep would be an important further development. It is important to solve issues with financial support such as asking authorities for re- sources, seeking grants for fundamental or clinical research.
Dr. Oana Deleanu shared the whole path of de- velopment beginning from far before 2008 when Romania was inspired by the German model of sleep education for doctors, and continuing to their final approval of model, which was done in 2011 in a form of the 3-module system – PG, PSG and positive airway pressure (PAP) titration, and was modified in 2013-2014.
She also stressed the importance of appropri- ate education and shared the teaching program for sleep professionals in Romania. The Romanian participants had to provide diplomas from sleep courses, perform respiratory PGs, and pass the examination by the European Respiratory Society handbook. The course consisted of 2 modules, in- cluding both theoretical parts and practical tasks, such as respiratory event scoring, performing PSG and PAP titration, discussing cases and ongoing is- sues. The diploma was awarded if the participant passed the final theoretical exam and successful- ly finished PSG scoring. As a result, from 2013 to 2019 their team prepared 169 sleep experts.
DR. LYUDMILA KOROSTOVTSEVA ABOUT SLEEP MEDICINE DEVELOPMENT EXPERIENCE IN RUSSIAN FEDERATION
Dr. Lyudmila Korostovtseva presented the “Sleep medicine, forming an interdisciplinary field – Russian Federation experience” topic. In her presentation she covered sleep disorders prevalence in Russia, identi- fying insomnia, EDS, and SDB as the most prevalent ones. She presented the main issues in sleep medi- cine development in Russia. The main problem was that sleep medicine is not recognized as a separate specialization or subspecialization, therefore no leg- islative and regulatory documents exist; in addition, there was a lack of sleep-related services and a lack of comprehensive educational programs either for sleep medical doctors or sleep technicians hamper the medical standards of health care.
Moreover, low awareness of physicians and pa- tients, together with low interest of hospital admin- istration and local authorities in the development of sleep medicine were also significant issues. Lyudmila Korostovtseva stressed the high costs of diagnostic and device-based other equipment and reimbursement issues as factors working against sleep medicine development.
Among other important issues, Lyudmila Korostovtseva brought an example of healthcare legislative documents regarding driving, where no screening for SDB and EDS was included in medical examinations. She recognized that cur- rently developing sleep medicine as a competen- cy area presents a possible approach in Russia. Although sleep medicine training programs are still in development, at some Russian medical univer- sities courses for undergraduate students are of- fered. Postgraduate education includes presenting sleep-related topics at annual medical meetings and short courses offered by some medical universities. As Russia is a large country, it is difficult to travel from one region to another. For this reason, online education via webinars and online educational presen- tations, and continuing medical education (CME) mod- ules work well for Russian clinicians. Widening the national sleep society network through journal pub- lications, guidelines for insomnia and OSA manage- ment, as well as education on a population level are
another ways of promoting sleep medicine in Russia.
PANEL DISCUSSION
During the discussion, the ANSS and ARSDA members gave recommendations based on dis- cussed topics. The main issues were the recogni- tion of sleep medicine as a (sub)specialization, or- ganizing proper education through undergraduate, postgraduate CME courses, seminars, and tailored workshops.
The round-table discussion participants were concerned about the absence of representatives of insurance companies and other authorities re- sponsible for driving licensing and other issues. Sleep disorders diagnostic and treatment reim- bursement involve a high economic burden which has to be solved by recognizing sleep disorders, and defining procedures as vital for patients. As EDS is an emerging issue among the Armenian population, there is a high risk of car accidents caused by falling asleep while driving or experi- encing a near-miss traffic accident. The other steps proposed to solve these issues were more focused meetings with the Police and the Ministry of Transport and Communication for further dis- cussion of this problem.
SDB treatment devices are not registered in Armenia as official non-pharmacological treatment options. The SCDMTE representative, Dr. Narek Baghdasaryan – a clinical pharmacologist, high- lighted this issue and offered to work on including CPAP, BPAP, and NIV as licensed SDB treatment options. This could help with easing the conditions of customs procedures and waving the taxes on their import which is currently done in Armenia.
The ANIH director Alexander Bazarchyan pro- posed to create an official statement paper with rec- ommendations included, which would be presented as a result of Round-table discussion and signed by the meeting organizers – ARSDA, ANSS, ANIH. This paper would be sent directly to the minister of health of Armenia and presented at the ANSS-ESRS meetings as a result of the “Beyond Boundaries” pi- lot project in Armenia.
THE ANSS-ARSDA-ANIH POSITION STATEMENTS AND RECOMMENDATIONS REGARDING SLEEPMEDICINE DEVELOPMENT IN ARMENIA
The ANSS-ARSDA-ANIH statements on current issues in sleep medicine in Armenia
► The participants recognize sleep disorders as a significant healthcare issue among the Armenian population. The prevalence study performed in Armenia showed a high incidence of insomnia, EDS, and SDB. The ARSDA states a high incidence of undiagnosed and misdiagnosed sleep disorders due to a low level of awareness among the gener- al population and healthcare professionals. Half of the Armenian population suffers from insomnia or poor sleep, there is a high number of participants with RLS. Smoking, obesity, hypertension, and di- abetes mellitus are widespread health issues inter- fering with sleep disorders.
► ARSDA and ANIH state that sleep medicine is not recognized as a separate field of healthcare, there is no mention of sleep medicine as a special- ization or subspecialization in the specialization list officially recognized by the MOH of Armenia. There is no unified system for sleep center accreditation, no standards for sleep laboratory equipment. Sleep medicine education in Armenia is nearly absent, and there is no special system to educate sleep techni- cians. The government of Armenia does not support sleep medicine professionals with grants or other means of aid for sleep research promotion, raising awareness by educating the general population and healthcare professionals.
► Due to the absence of a reimbursement sys- tem, the sleep-disorders-related costs are a big public health burden in Armenia. The diagnosis and treatment of sleep disorders are associated with high costs and patients tend to avoid excessive expenses due to low socioeconomic status and the absence of comfortable insurance services.
► There is a need for better education of gen- eral practitioners and narrow specialists in sleep disorders and their role in their respective fields to increase referrals for their diagnosis.
The ANSS-ARSDA-ANIH recommendations for improvement of sleep medicine in Armenia
► The ANSS-ARSDA-ANIH encourage the rec- ognition of sleep medicine as an autonomous field of healthcare within a set of several main clinical specialties (neurology, pulmonology, cardiology, psychiatry, etc.) in Armenia. Sleep medicine should be accepted as a specific field of clinical practice by the Armenian MOH and confirmed by the govern- ment of Armenia.
► The ANSS-ARSDA-ANIH recommend creat- ing and developing modules, qualification, and fel- lowship programs for Armenian medical students, residents from different relevant specialties, and healthcare professionals willing to be involved in sleep disorders management. The recommenda- tion includes creating a list of specialties eligible for studying sleep medicine and developing educa- tional programs.
► As a provider of accreditation of medical edu- cation programs in Armenia, ANIH encourages and admits the possibility of including sleep medicine in professional medical education by organizing studies within undergraduate and postgraduate programs also including sleep medicine topics in the framework of CME.
► The ANSS-ARSDA-ANIH recommend pro- moting accreditation of sleep centers and sleep professionals, certification of sleep technicians (and EEG-technicians as a related profession). The accreditation of sleep centers should involve the development of legislative documents with stan- dards of practice for sleep laboratory equipment. Sleep professionals and sleep technicians should undergo certification and accreditation processes by ANIH standards.
► The ANSS with the help of the ESRS endorses continuing sleep medicine education and supports the improvement of professional knowledge on the international level via regular ESRS congresses, teaching courses, professional visits to Armenia, and participation in online teleconferences, and other educational opportunities.
► The ANSS-ARSDA-ANIH recommend includ- ing main sleep disorders in the national statistical registries of disorders in Armenia.
► The ANSS and ARSDA recommend proceed- ing with the identification of the list of important sleep-related drugs, absent from official registration on the territory of Armenia. This list should be included in the negotiations with various organiza- tions for making at least some of them available in Armenia for adequate sleep practice.
► The ANSS-ARSDA with the encouragement from a representative of SCDMTE, the national drug regulatory agency, recommend working on formal regulations for the non-pharmacological treatments of respiratory sleep disorders, such as CPAP, BPAP, NIV, and others. The agency supports the idea and its quick implementation.
► ARSDA states the need for governmental support for NGOs for the general population and healthcare professional education. ARSDA with the help of ANSS and ANIH will translate, adapt and develop guidelines for sleep disorders manage- ment among Armenian physicians.
► The ANSS-ARSDA-ANIH state the need for reimbursement for sleep diagnostic studies and treatment. Insurance companies, MOH, and other authorities should discuss and include sleep disor- ders management-related costs within the list of compensated services.
► ARSDA will provide ANIH with sleep disor- ders prevalence data, which will be spread among medical professionals. Research in sleep medicine should be promoted and encouraged by ANIH, MOH, and the Armenian Government.
► The ANSS-ARSDA-ANIH endorse the devel- opment of legislative and regulating documents for driving license issuing, regular screening of drivers for sleep disorders particularly for excessive day- time sleepiness, and sleep attacks in long-distance drivers. The recommendation includes the devel- opment of standards for obstructive sleep apnea and excessive daytime sleepiness screening among drivers by using PG, PSG and MSLT/MWT.
► ARSDA recommends highlighting insomnia, sleep-disordered breathing issues, educating the population on the physiologic nature of behavioral sleep disorders to destigmatize patients with sleep- walking, nocturnal epilepsy, and sleep enuresis, teaching the general population on how to sleep and improving sleep hygiene, promoting non-phar- macological treatments for sleep disorders such as CBT-I, CPAP, BPAP, etc. With all this progress moving sleep medicine to a more commercial level will also stimulate the development of this field in Armenia.
CONCLUSION
There is a great need to fill the gap between the highly important role and big impact the various sleep disorders have on public health and clinical practice. In addition, there is a dearth of attention from medical and government authorities, finan- cial support, and inclusion in various educational and insurance programs. The current article rep- resents an important milestone in summarizing the round-table discussion with European body rep- resentatives to identify the problems in Armenian sleep medicine and suggest solutions targeting the improvement of sleep practice in Armenia in vari- ous ways.
ACKNOWLEDGEMENTS
The ANSS EC and ARSDA would like to express their appreciation to the ANIH and MOH of Armenia for hosting the meeting and raising the awareness to a higher level of recognition.
REFERENCES
- Patel D., Steinberg J., Patel P. Insomnia in the elderly: a review. J Clin Sleep Med. 2018;14(6):1017-1024.
- Sweetman A., Lack L., Bastien C. Co-morbid insomnia and sleep apnea (COMISA): prevalence, consequences, methodological considerations, and recent randomized controlled trials. Brain Sci. 2019;9(12):371.
- Matsumoto T., Chin K. Prevalence of sleep disturbances: sleep disordered breathing, short sleep duration, and non-restorative sleep. Respir Investig. 2019;57(3):227-237.
- Dopheide J.A. Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am J Manag Care. 2020;26(4S):S76-S84.
- American Academy of Sleep Medicine. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago, Illinois: American Academy of Sleep Medicine; 2001.
- World Health Organization. ICD-10: international statistical classification of diseases and related health problems: 10th revision, 2nd ed. World Health Organization; 2004.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). 2013.
- Khachatryan S.G., Ghahramanyan L., Tavadyan Z., Yeghiazaryan N., Attarian H.P. Sleep related movement disorders in a population of patients with epilepsy: prevalence and impact of restless legs syndrome and sleep bruxism. J Clin Sleep Med. 2020;16(3):409-414.
- Andrade A.G., Bubu O.M., Varga A.W., Osorio R.S. The relationship between obstructive sleep apnea and Alzheimer’s disease. J Alzheimers Dis. 2018;64(s1):S255-S270.
- Mullins A.E., Kam K., Parekh A., Bubu O.M., Osorio R.S., Varga A.W. Obstructive sleep apnea and its treatment in aging: Effects on Alzheimer’s disease biomarkers, cognition, brain structure and neurophysiology. Neurobiol Dis. 2020;145:105054.
- Ju Y E S, Videnovic A, Vaughn B V. Comorbid sleep disturbances in neurologic disorders. Continuum (Minneap Minn). 2017;23(4, Sleep Neurology):1117-1131.
- Khachatryan S.G., Tavadyan Z.D., Margaryan H.S., Mouradyan H.S., Zelveian P A. O0040 Prevalence of restless legs syndrome in the general adult population of Yerevan, Armenia. Sleep Medicine. 2007;8:S57-S58.
- Dikeos D., Georgantopoulos G. Medical comorbidity of sleep disorders. Curr Opin Psychiatry. 2011;24(4):346-354.
- Wang Q., Wang X., Yang C., Wang L. The role of sleep disorders in cardiovascular diseases: Culprit or accomplice? Life Sci. 2021;283:119851.
- Nigam G. Camacho M., Chang E.T., Riaz M. Exploring sleep disorders in patients with chronic kidney disease. Nat Sci Sleep. 2018;10:35-43.
- Braley T.J., Boudreau E.A. Sleep disorders in multiple sclerosis. Curr Neurol Neurosci Rep. 2016;16(5):50.
- Krystal A.D. Psychiatric disorders and sleep. Neurol Clin. 2012 ;30(4):1389-1413.
- Khurshid K.A. Comorbid insomnia and psychiatric disorders: an update. Innov Clin Neurosci. 2018;15(3-4):28-32.
- Hirshkowitz M., Whiton K., Albert S.M. et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43.
- Watson N.F., Badr M.S., Belenky G. et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. J Clin Sleep Med. 2015;11(8):931-952.
- Silva A.A., Mello R.G.B., Schaan C.W., Fuchs F.D., Redline S., Fuchs S.C. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open. 2016;6(2):e008119.
- Lavie P., Lavie L., Herer P. All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J. 2005;25(3):514-520.
- Yazdan-Ashoori P., Baranchuk A. Obstructive sleep apnea may increase the risk of stroke in AF patients: refining the CHADS2 score. Int J Cardiol. 2011;146(2):131-133.
- Isayan M., Hovakimyan H., Khachatryan S. The prevalence of sleep-related car accidents in Armenia. In: J Sleep Res. 2020;29:189-190.
- Wang X., Cheng S., Xu H. Systematic review and meta-analysis of the relationship between sleep disorders and suicidal behaviour in patients with depression. BMC Psychiatry. 2019;19(1):303.
- Bernert R.A., Hom M.A., Iwata N.G., Joiner T.E. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J Clin Psychiatry. 2017;78(6):e678-e687.
- Taddei-Allen P. Economic burden and managed care considerations for the treatment of insomnia. Am J Manag Care; 2020:26(4S):S91-S96.
- Watson N.F. Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. J Clin Sleep Med. 2016;12(8):1075-1077.
- Walia H.K., Thompson N.R., Katzan I., Foldvary-Schaefer N., Moul D.E., Mehra R. Impact of sleep-disordered breathing treatment on quality of life measures in a large clinic-based cohort. J Clin Sleep Med. 2017;13(11):1255-1263.
- Ishak W.W., Bagot K., Thomas S. et al. Quality of life in patients suffering from insomnia. Innov Clin Neurosci. 2012;9(10):13-26.
- Penzel T., Pevernagie D., Bassetti C. et al. Sleep medicine catalogue of knowledge and skills – Revision. J Sleep Res. 2021;30(3):e13394.
- Bylaws. European Sleep Research Society/ Assembly of National Sleep Societies https://esrs.eu/about/bylaws/. Accessed August 28, 2021.
- Khachatryan S., Ghahramanyan L., Stepanyan A. et al. Prevalence of sleep disorders in the adult population of Armenia: an epidemiological study. In: J Sleep Res. 2020;29:91.
- Sleep and Sleep Disorder Statistics. American Sleep Association. https://www.sleepassociation.org/about-sleep/sleep-statistics/. Accessed August 14, 2021.
- Voinescu B.I. Common sleep, psychiatric, and somatic problems according to work schedule: an internet survey in an Eastern European country. Int J Behav Med. 2018;25(4):456-464.
- Kansagra S. Sleep Disorders in Adolescents. Pediatrics. 2020;145(S2):S204-S209.
- Ophoff D., Slaats M.A., Boudewyns A., Glazemakers I., Van Hoorenbeeck K., Verhulst S.L. Sleep disorders during childhood: a practical review. Eur J Pediatr. 2018;177(5):641-648.