Mukuchyan V.,1, Bdoyan G.,2 Mkhitaryan E.,2 Mardyan A.1
1Service of rheumatology and immunology, Nairi Medical Center, Yerevan, Armenia
2Department of orthopedics and traumatology, Erebouni Medical Center, Yerevan, Armenia
ABSTRACT
Introduction: Paget’s disease is a disorder of bone remodeling that typically begins with excessive bone resorption followed by an increased bone formation. This misbalance into new bone formation process and osteoclastic activity leads to a structurally disorganized mosaic of bone, which is mechanically weaker, larger, less compact, more vascular, and more susceptible to fracture than normal adult bone.
Case description: We report the case of a 66-year-old woman who came to us due to a nonunion two months after surgical fixation of the right femoral neck fracture. Upon admission, a pelvic radiograph revealed right femoral neck fracture with osteolysis. A biopsy of the greater trochanter demonstrated histopathological patterns of Paget’s disease. After the surgical intramedullary metallic osteosynthesis of the femoral neck, the patient left the hospital suggested for physiotherapeutic treatment with quadriceps isometric exercises. After 2 months, the pelvic X-ray revealed absence of callus, and the patient was referred to a rheumatologist. Intravenous administration of bisphosphonates (zoledronic acid), as well as oral intake of calcium and vitamin D has been prescribed.
Conclusions: Besides rheumatologists and endocrinologists, clinical recognition of Paget’s disease is also very important for orthopedic surgeons in order to achieve better results for patients suffering from any kind of major osteoporotic fracture.
Keywords: Paget’s disease, hip fracture, nonunion, osteoporosis
DOI:10.54235/27382737-2021.v1.2-52
INTRODUCTION
Paget’s disease was first described in 1877 by Sir James Paget, a British surgeon who named the condition “osteitis deformans,” as he believed the disease was caused by chronic inflammation.[1] Today the disease is characterized as a disorder of bone remodeling that typically begins with excessive bone resorption, followed by an increase in bone formation. This misbalance into new bone formation process and osteoclastic activity results in a structurally disorganized mosaic of bone, which is mechanically weaker, larger, less compact, more vascular, and more prone to fracture than normal adult bone. All bones may be affected to varying degrees.[2] Complications such as neurological deficits and cardiac failure, arthritis, hearing loss, and rarely, osteosarcoma may also occur.
CASE DESCRIPTION
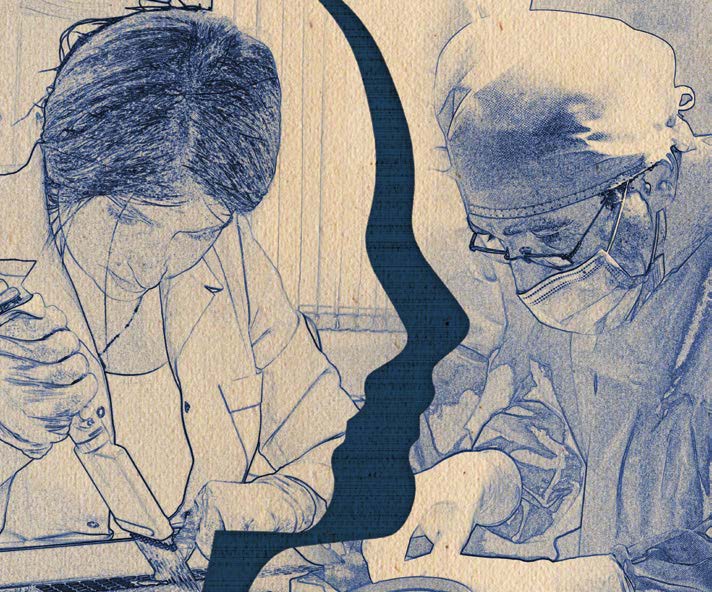
A 66-year-old female was admitted to the emergency room by ambulance complaining of pain in right lower extremity and limited range of motion. Symptoms began after trauma from a fall. The pelvic radiograph revealed right femoral neck fracture with characteristic bone osteolytic and osteosclerotic lesions (Fig. 1, 2 and 3).
The menopause developed 15 years ago. She had no history of joint or bone pains, deafness, dental malocclusion, fractures or body weakness. She had not noticed any abnormal enlargement of the bones of her body, neither history referable to the cardiovascular system. The past medical history was negligible with no known family history of bone disease. She had never been prescribed calcium or vitamin D supplements. A biopsy of the greater trochanter was performed due to an unusual X-ray, revealing histopathological patterns of Paget’s disease. The patient underwent surgical intervention of intramedullary metal osteosynthesis of the right femur (Fig. 4).
During hospitalization, blood calcium, alkaline phosphatase (ALP = 69.53 U/L; reference range, 40-130), parathyroid hormone and phosphorus levels were within normal ranges, but vitamin D level was significantly reduced (11.2 ng/dL; reference range, 30-70). On the fifth day after an uneventful surgical intervention, the patient was discharged from the inpatient clinic with suggestions to continue physiotherapeutic treatment with quadriceps isometric exercises. At 2-month follow-up, the pelvic X-ray revealed the absence of callus, and the patient was referred to a rheumatologist (Fig. 5).
At the rheumatology clinic, all blood tests were normal, except the elevated level of ALP (248.76 U/L; reference range, 40-130) and a decreased level of vitamin D (10.9 ng/dL; reference range, 3070). Treatment with intravenous bisphosphonate (zoledronic acid 4 mg), calcium 1200 mg/day, vitamin D 50.000 IU/week and nonsteroidal anti-inflammatory drugs was started. The patient is under close follow-up.
DISCUSSION
Paget’s disease is the second most common bone disease after osteoporosis. Its’ prevalence shows wide geographical variation, common in Western Europe, Americas, and Australia, but rare in Asia and Africa. However, recent studies have reported an unexplained reduction in both prevalence and disease severity.[3] Genetic factors are clearly an important component of the etiology of Paget’s disease, since 15-40% of affected patients have a first-degree relative with Paget’s disease.[4] Many signs and symptoms characteristic for clinical or radiological changes in Paget’s disease have been described in the past. The “Lincoln sign” or “black beard” sign could be found when the disease involved the mandible. The “osteoporosis circumscripta”. The “Tam O’Shanter skull” and the classic “cotton wool” appearance of the bone are the most well-known radiological signs of Paget’s disease. The “blade of grass” or “flame sign” in the long bones, thickened pelvic brim known as the “brim sign” and the “picture frame,” “double contour” or “windowed” vertebral body are other radiological patterns of the disease.[5] Certain biochemical markers could be increased like: ALP, osteocalcin, serum N-telopeptide of type I collagen, serum C-telopeptide of type I collagen and serum deoxypyridinoline cross-links of type I collagen.[6] The main complication of the disease is bone fractures. The current mainstay treatment for Paget’s disease is bisphosphonates, which are also largely used to treat osteoporosis. Adequate calcium and vitamin D supplements should be given to achieve the desired result. Although there are no studies yet to support whether treating asymptomatic patients with Paget’s disease with subsequent normalization of ALP actually reduces the complications in the long term.
Fig. 1. Deformation and osteoporotic changes of the right femoral head (CT scan).
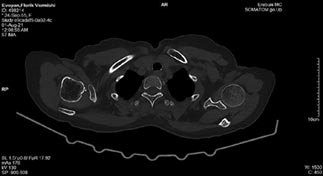
Fig. 2. Osteolytic and osteosclerotic changes of the right femoral head and neck (CT scan).
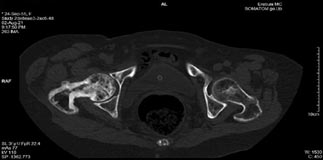
Fig. 3. Right proximal femoral (hip) fracture (CT scan).

Fig. 4. X-ray image of the right femur 5 days after the intramedullary metal osteosynthesis showing appropriate repositioning.

Fig. 5. X-ray image of the right femur 5 days after the intramedullary metal osteosynthesis showing appropriate repositioning.

CONCLUSIONS
In addition to rheumatologists and endocrinologists, clinical recognition of Paget’s disease is also crucial for orthopedic surgeons in order to achieve better results for patients suffering from any kind of major osteoporotic fracture. In the initial stages, the disease may be asymptomatic, but it can be diagnosed with pathognomonic radiological and serological features that can help prevent potential serious complications of the disease.
Declaration of interest: The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding: This research did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Patient consent: A written informed consent has been obtained from the patient.
REFERENCES
- Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2:177-202.
- Lalam RK, Cassar-Pullicino VN, Winn N. Paget disease of bone. Semin Musculoskelet Radiol. 2016;20(3):287-299.
- Bastin S, Bird H, Gamble G, Cundy T. Paget’s disease of bone: becoming a rarity? Rheumatology (Oxford). 2009;48:1232-1235.
- Karunakaran K, Murugesan P, Rajeshwar G, Babu S. Paget’s disease of the mandible. J Oral Maxillofac Pathol. 2012;16:107-109.
- Bhargava P, Maki JH. Images in clinical medicine. “Cotton wool” appearance of Paget’s disease. N Engl J Med. 2010;363:e9.
- Roodman GD, Windle JJ. Paget disease of bone. J Clin Invest. 2005;115:200-208.