INTRODUCTION
Medical activity has a thousand-year history, and alongside it, the processes of regulation and control of this activity have evolved and improved. In all developed countries, the medical profession requires a national license to identify qualified professionals. We conducted a survey and carried out a comparative analysis of events occurring in this domain across various countries and periods, as well as the current situation and potential developments in Armenia.
Historical Overview
The activities of doctors have been regulated since time immemorial. Licensing of doctors and implementing restrictions on their unauthorized activities have a lengthy history, making them not exclusive to modern society. Prior to the utilization of contemporary tools for assessing knowledge and skills, diverse methods were used to regulate medical practice. Even in the Old Testament, numerous references exist on whom to approach healing and how. The regulation of medical activity likely commenced around 4000-5000 years ago. For instance, Homer praised Egyptian doctors as experts with specialized skills.
The process of regulating medical practice in the United Kingdom began in 1421 during the reign of Henry V. However, the necessary laws were enacted later, during the rule of Henry VIII. Seven acts of parliament are described, outlining requirements for medical practice and licensing of doctors, as well as entities and institutions responsible for imposing these licensing requirements. Despite some unsettled legal aspects of medicine, no further legislation was passed in England until 1858, when the Medicine Act was enacted. [1]
The history of the regulation of medical activity in the United States developed alongside the formation of America. In New York in 1684, the adoption of colonial law established that the practicing medicine “without the consent of specialists in the specified field” was prohibited. In 1649, in Massachusetts, physicians and surgeons were barred from treating without “the advice and consent of a specialist in the same field.” In 1870, state medical commissions began forming, granting approval for professional activities. By 1978, the State Medical Boards ceased to exist, and federal licensing and national boards became the standard for professional practice. In 1992, the Medical Licensing Examinations were introduced for the first time. [2]
In the Russian Empire, Peter I attached great importance to education and advancement of medicine. During his reign, the first medical center and medical school were founded in 1706 and 1707. In 1832, Nicholas I set a deadline for submitting a package of legislative acts. This year marked the presentation of the “Collection of Laws of the Russian Empire,” which included legal norms in the healthcare domain. Over the years, new chapters were added to this legislative compilation. The chapter “On Doctors” contained norms regulating the distribution of doctors, procedures for their appointment to positions, responsibilities of doctors in urban and rural areas, as well as special provisions for specialists lacking certificates or diplomas from Russian medical schools to prevent them from treating patients. [3]
In Armenia: 301 AD – adoption of Christianity as the state religion. About 100 years later, in 405 AD, the Armenian alphabet was invented, and the extensive experience gained in traditional medicine served as the foundation for the establishment and development of scientific medical system in Armenia. Alongside the construction of churches and monastic complexes, the first hospitals were established. In 365 AD, a decision of the church assembly declared: “To prevent the spread of contagious diseases, establish leper colonies, hospitals for the sick, and shelters for the disabled.” During the Armenian medieval revival (10th to 14th centuries), medical science also experienced rapid development. Medieval academies were established, offering instruction in medicine alongside other disciplines. Moreover, the great teachers of that era highly valued practical knowledge. Notably, Hovhannes the Deacon (1045-1129) stated: “Knowledge cannot be accurate without experience.” Historical records affirm the existence of a healthcare system that took shape and developed in Ani, the capital of Armenia during this period. The established healthcare system and wealth of accumulated literature facilitated the training of doctors and the transmission of knowledge across generations, often through apprenticeship with renowned doctors in monastic academies. Additionally, it is worth mentioning that the works of many Armenian doctors encompass not only medical teachings but also descriptions and definitions of the image of a doctor – a professional imbued with a profound sense of duty and lofty moral standards. [4]
Current Situation in the World
In the modern world, the regulation of doctors’ professional activities is accomplished through state licensing exams. These exams align with the requirements of a given country’s healthcare system and established standards. In the USA, Great Britain, Germany, Spain and several other European countries, mechanisms exist for evaluating the competence of a medical professional. These mechanisms assess the level of knowledge and skills of medical workers, ensuring their adherence to the prevailing standards in the country. A number of countries consider the existence of documents confirming the fact of their education (e.g., the Netherlands), some countries regard possessing a license (e.g., the USA) as requisite for entry the healthcare sector. Frequently, the licensing process coincides with the registration in the medical professionals’ registry. The authority overseeing licensing also varies; for instance, in Malta, professional medical associations handle licensing and registration, whereas in Estonia, it is managed by state authorities. [5]
In general, the regulation of health workforce potential involves regulating and controlling processes during education, entry into the healthcare sector, and engagement in healthcare activities. During medical education, factors such as duration, content, format of education programs, and accreditation of educational institutions may be standardized and supervised. Upon entering the healthcare sector, medical professionals must validate their eligibility to practice, typically through licensing and/or registration. This validation can be issued for the entire period of professional career or renewed periodically (relicensing). When providing medical services, medical personnel must ensure the continual upkeep of their competencies and engage in continuous professional development (CPD). At each stage, various strategies or mechanisms can be implemented to prevent the entry or involvement of unqualified personnel in the system. Furthermore, these strategies should be harmonized as closely as possible with government policies and global health goals.
Situation in Armenia
In the 1960s, during the Soviet era in Armenia, the concept of continuous education for medical specialists and a system for enhancing their skills were introduced and operated for decades. Subsequently, following Armenia’s newfound independence, a system for postgraduate additional education of medical specialists was established based on this foundation. This system was enshrined in the law on postgraduate education, which also mandated medical specialists to undergo mandatory training every 5 years. In order to maintain the continuity of their professional practices, doctors were required to complete 7 weeks of training, while nurses were expected to complete 5 weeks of training.
Towards the late 1990s, Armenia introduced an individual licensing system for medical professionals. This involved a computerized test exam and the issuance of an individual professional license for medical practitioners. However, in 2001, the individual licensing system for medical professionals in Armenia was suspended. This was mainly due to the understanding that medical care and services, categorized by type, are organizational issues within the medical facility, rather than the sole responsibility of an individual doctor. The focus shifted to the staffing and equipping of medical facilities, rather than solely emphasizing the professional competences of individual doctors.
The mandatory training system model remained relevant until 2016, when wording was added to the RA Law “On Medical Assistance and Services to the Population” that aligned with the CPD certification model for medical practitioners. This model entails medical specialists accumulating a specific number of Continuous Medical Education (CME) credits within a 5-year cycle. Confirmation of 3 years of professional work experience during the specified cycle was also required, which was the basis for issuing a certificate of independent professional activity. Newly graduating specialists were eligible for the “Certificate of professional activity for the first time”, which was issued to clinical residency graduates and valid for 5 years. During this 5-year period, healthcare professionals who were already providing healthcare services were obligated to accumulate the amount of CME credits mandated by law and apply for a professional practice certificate. Doctors needed to acquire 220 credits within a 5-year cycle, nurses were required to attain 140 credits. Hence, in 2016, the changes were scheduled to take effect from January 1, 2020. However, the COVID-19 pandemic introduced its own “regulations” into the functioning of the healthcare system, leading to the revision of the terms for certification of medical practitioners. The new certification term for medical professionals was rescheduled to start on January 1, 2023.
Simultaneously, an attempt was made to leverage the change in the term to benefit medical professionals. This calculation cycle covered the period from 2016 to 2022. If a medical worker failed to accumulation of required number of credits or lacked the necessary professional work experience within the specified period, they had the option to participate in a computer-based testing exam and would receive a certificate upon achieving a positive result. In 2022, packages containing documents from more than 30,000 medical specialists were submitted to the National Certification Center for Professional Development (NCCPD). Upon initial review, these packages were forwarded to professional commissions established by the Ministry of Health. Medical professionals were provided the option to submit documents electronically. By January 1, 2023, a substantial portion of the medical specialists of Armenia confirmed their eligibility for independent professional activity by acquiring certificates of professional activity. It is important to note that specialists who entered the healthcare sector after completing clinical residency (ordinatura) also obtained “First-time professional activity” certificates. These certificates were granted on documents indicating the completion of clinical residency and a state diploma.
The process of organizing the certification of medical specialists revealed that despite the existing legal requirement to ensure the availability of professional training, considerable number of medical workers did not receive the necessary amount of training. Indirect evidence of this lies in the unprecedented surge in the number of trainings observed in 2022. The certification process also highlighted various organizational and legal issues that served as the impetus for initiating legislative changes.
The current certification system in Armenia only permits a documentary assessment of the ongoing development of medical practitioners. Standardized approaches within the medical education system are lacking, and there is no evaluation and oversight of the competencies of the established human resources by independent bodies. One plausible solution to these and several other challenges related to the human resources potential of healthcare could be the implementation of an individual licensing system. The prospect of introducing this new initiative is motivated by:
• Ensuring the availability of competent human resources to the health sector.
• Lack of monitoring and control mechanisms to gather information on the quality of human resources.
• The necessity to define and broaden the scope of medical services provided by clinical residents, alongside their authority within healthcare facilities.
• Lack of a control system and administrative accountability mechanisms in case of ethical rule violation by medical staff, which would allow learning about cases and circumstances of violations, analyze and correct them.
To initiate the process, a series of discussions were organized with the participation of leading experts in the field, representatives from educational institutions, and a study of international experience and best practices. Based on these, a package of legislative acts was developed and sent to all relevant departments through the prescribed procedures. The proposed licensing system model includes integrating personnel potential into the healthcare system and implementing mechanisms for assessing and monitoring the competencies of the existing potential within the system. It is recommended that candidates for clinical residency be granted licenses with the possibility of obtaining licenses with certain limited powers, which would be followed by the issuance of a foundational license upon residency completion. In both scenarios, the issuance a license is contingent on achieving positive results in centralized examinations. Competence maintenance and license renewal within the healthcare field will be based on accruing a certain number of CME credits and having a clean record devoid of disciplinary or ethical violations. The presented model actually covers both entry and activity in the medical services sector.
The reimplementation of licensing system is scheduled according to the scheme presented in Figure 1. Medical graduates from all medical institutions, whether public or private, who pass the relevant licensing exam, will be granted a Transitional license. This license will enable them to obtain a certain status and work in a medical organization under faculty supervision, with remuneration during their residency. Upon completing their residency and successfully passing the requisite licensing exam, medical professionals will be issued their license, valid for 5 years. A requirement for relicensing will be the accumulation of specified number of CME credits and the absence of disciplinary and ethical violations.
SURVEY
Along with the start of work on the introduction of the licensing system, there was a need for wider discussions involving a larger number of medical professionals. An anonymous survey was conducted to gather opinions and recommendations from these professionals. An electronic survey questionnaire comprising 14 questions was developed. A link to the electronic questionnaire was distributed to diverse departments of the Ministry of Health, advisers to the Minister of Health, representatives of educational institutions, regional health departments, heads of medical institutions and medical workers.
A total of 332 specialists took part in the survey, with an age ranged between 24 and 73 years. Among them, 225 (68%) participants were women, 107 (32%) were men. More than half (56%) of the survey participants stated that they are aware of the work carried out towards the introducing a licensing system for medical workers. An analysis of the responses regarding the professional orientation of the participants revealed that specialists from almost all areas, whether surgical or therapeutic, as well as representatives of management and educational entities, participated in the survey. An analysis of the question about the positions occupied by the participants showed that the survey involved primary healthcare workers and hospital units, representatives of the administrative-territorial structure of medical institutions, department heads, consultants of the Ministry of Health and representatives of various departments of the Ministry of Health. A significant majority, 323 (97%) respondents, agreed with the statement that the competence of medical personnel plays a key role in the performance of the health sector. When asked about the most critical factor for ensuring healthcare system quality, respondents’ priorities are depicted in Figure 2: 27% of respondents answered ‘yes’, 13% answered ‘no’, 57% answered partially. Regarding ensuring the continuous alignment of medical education with modern requirements of the services provided, participants’ preferences were distributed as follows: 33% proposed addressing the issue through the development and implementation of modern guidelines and protocols, 41% through continuous training of medical professionals, 26% through testing the knowledge and skills of medical practitioners. Additionally, 45% of respondents suggested assessing knowledge levels based on CME credits, while 55% preferred regular exams. The opinions of survey participants regarding the most effective method of testing knowledge were distributed as follows: 43% of participants believed a combination of oral and written exams to be most effective, 36% favored written exams only, and 12% preferred oral exams. The distribution of opinions among survey participants regarding the assessment of practical skills in medical personnel is shown in Figure 3.
DISCUSSION
In our opinion, the survey effectively covered a broad spectrum of stakeholders in the process. Additionally, the survey indirectly contributed to enhancing the medical community’s awareness of the ongoing efforts, as the number of emails sent exceeded the actual number of survey participants by times. Even those health professionals who received the message but did not participate in the survey gained insight into the survey’s purpose. The age distribution of respondents also indicates the participation of representatives from various generations within the medical community. Only 24% of the survey participants indicated that the introduction of a system for licensing medical professionals would not enhance human resources and service quality (Figure 4). Interestingly, the supporters of this viewpoint were primarily medical professionals, while administrative and educational circles were notably less inclined to oppose the licensing system. This divergence might stem from medical specialists perceiving additional inconvenience with the system’s introduction and not fully welcome the assessment of their knowledge and skills. Therefore, efforts should be directed towards increasing the willingness of healthcare specialists and engaging them.
The survey participants presented a variety of recommendations for the smooth process organization and implementation. They also highlighted potential obstacles, which we endeavored to summarize and categorize as much as possible. Despite the fact that some of the survey participants see no obstacles to the introduction of the licensing system, the majority of medical professionals expressed concerns regarding its resumption. These concerns primarily revolve around possible deficiencies in the organization of the process, specifically:
• The necessity and timing of initiating the process.
• Adequate organization of the examination, ensuring sufficient and relevant examination materials for the country’s requirements.
• The impartial functioning of the commissions, including mitigation of potential corruption risks.
• Potential financial challenges, especially for medical personnel working in regions.
Survey participants propose addressing the aforementioned potential issues through the study of foreign experiences, competent planning and organization of the process, engagement of knowledgeable specialists, expansion of the national methodological recommendations database, implementation of a multi-level control system, provision of preparatory opportunities for medical personnel, and judicious timing for initiating and conducting the process.
CONCLUSION
Undoubtedly, ensuring the management of the process of formation of health personnel potential is one of the components of ensuring the quality of formation of this potential. However, the mechanisms for its implementation can vary in terms of structure and content. The organization and implementation of this process encompass various segments of the healthcare and education systems: medical educational institutions, entities responsible for accrediting educational institutions, healthcare policy makers, accrediting bodies for medical professionals, and, naturally, medical practitioners themselves. This complexity underscores the multi-layered nature of process and its broad range of stakeholders.
We believe that the outcomes of our study have effectively captured the opinions and recommendations of healthcare representatives regarding the implementation of a licensing system for medical professionals in Armenia. These findings can contribute to a smoother organization of the process.
REFERENCES
- Hughes JT. The licensing of medical practitioners in Tudor England: legislation enacted by Henry VIII. Vesalius. 2006;12(1):4-11
- A Brief History of the Regulation of Medical Practice: Hammurabi to the National Board of Medical Examiners Claudio Violato, PhD, Wake Forest School of Medicine. imerg.org/wp-content/uploads/2016/08/Violato-2016-History-of-medical-practice.pdf. Accessed: 25 December 2023
- A review of this period is given in an article on “Medical Education in Soviet Russia,” by Dr. W. Horsley Gantt, in the British Medical Journal, June 14, 1924. marxists.org/archive/newsholme/1933/red-medicine/ch17.htm#body-1. Accessed: 25 December 2023
- Vardanyan S. History of medicine in Armenia: from ancient times to present days. Yerevan, 2000.
- Kreutzberg A, Reichebner C, Maier CB et al. Regulating the input: health professions. In: Busse R, Klazinga N, Panteli D et al. (eds). Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.) 5. ncbi.nlm.nih.gov/books/NBK549267. Accessed: 25 December 2023
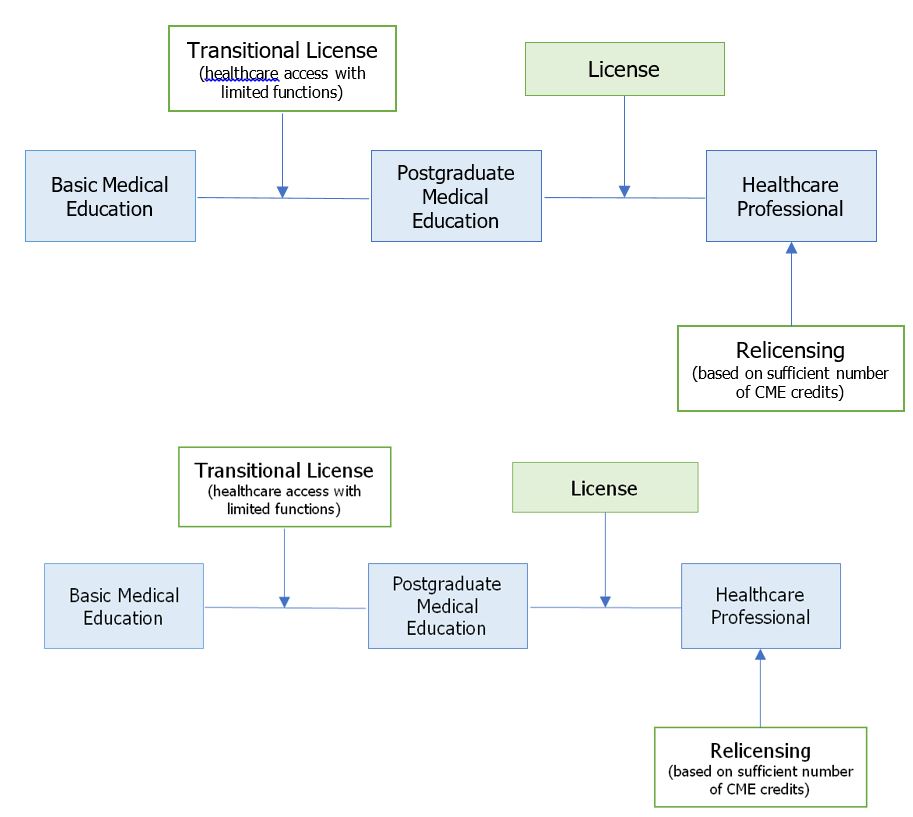
Figure 1․ Schematic illustration of the proposed model of licensing of healthcare professionals in Armenia

Figure 2. Distribution of opinions of survey participants regarding the components of quality assurance in the healthcare system in Armenia
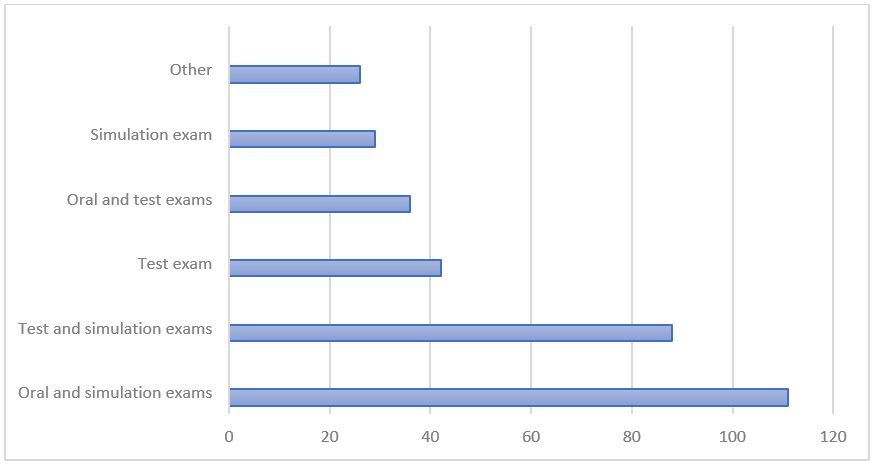
Figure 3. Distribution of opinions of survey participants regarding the most effective way of practical skills assessment among medical workers in Armenia
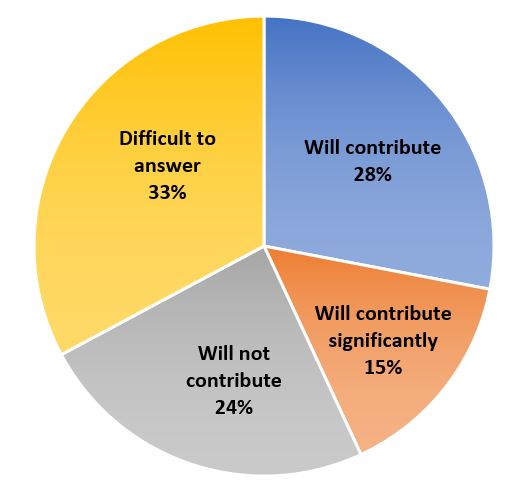
Figure 4. To what extent will the introduction of the licensing system contribute to the improvement of human resources and the quality of services provided in Armenia