INTRODUCTION
The brain lymphoma, also known as primary cerebral lymphoma or primary central nervous system lymphoma is a rare, highly aggressive non-Hodgkin cancer with an incidence of 0.5/100,000 inhabitants per year [1]. If detected early, it can be treated or even cured [2].
We present a case of histologically confirmed large B-cell lymphoma. The diagnosis was strongly suspected through perfusion magnetic resonance imaging (MRI) and magnetic resonance spectroscopy (MRS).
CASE PRESENTATION
A 42-year-old male patient developed unusual, sudden-onset, bilateral and afebrile headaches for 5 days. His family described the appearance of apathy and hypersomnia. Otherwise unremarkable medical history.
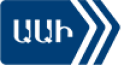
Figures 1, 2 and 3 show the computed tomography, MRI and MRS images, respectively.
DISCUSSION
Primary cerebral lymphomas have specific characteristics on perfusion MRI and MRS [3], such as:
► typical appearance of blood-brain barrier rupture with a rise of the baseline in perfusion
► no arguments for neoangiogenesis with the study of cerebral blood volume
► spectroscopic profile with an increase of the choline/N-acetyl aspartate (NAA) and choline/creatinine ratio. Also a lipid-lactate peak.
However, it is important to remember that 25% of primary cerebral lymphomas do not have this typical radiological profile. [4]
This is why histological proof is requested in most cases although it is not necessary when typical brain imaging is found associated with a positive vitreous sample (cytology, immunophenotyping and molecular biology) or a positive cerebrospinal fluid sample (cytology and flow cytometry).
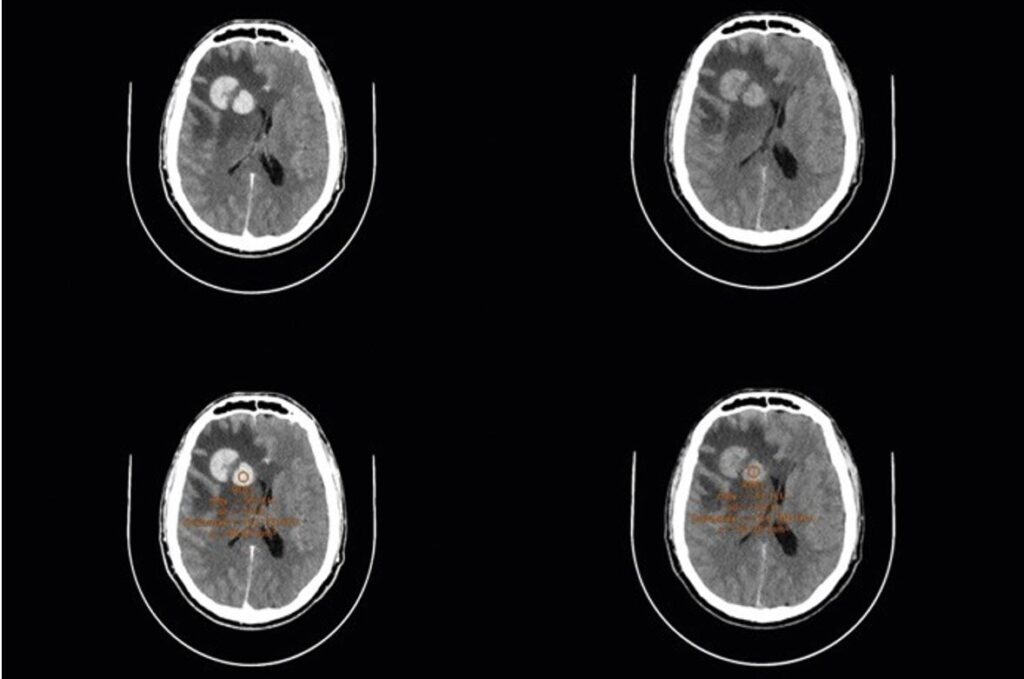
Fig. 1. Computed tomography without (A) and with (B) injection. Right frontal lesion in spontaneous hyperdensity (A). The injection shows an enhancement of the lesion (B), excluding a hemorrhagic process. Digitiform right temporofrontal edema with moderate mass effect on ventricular system.
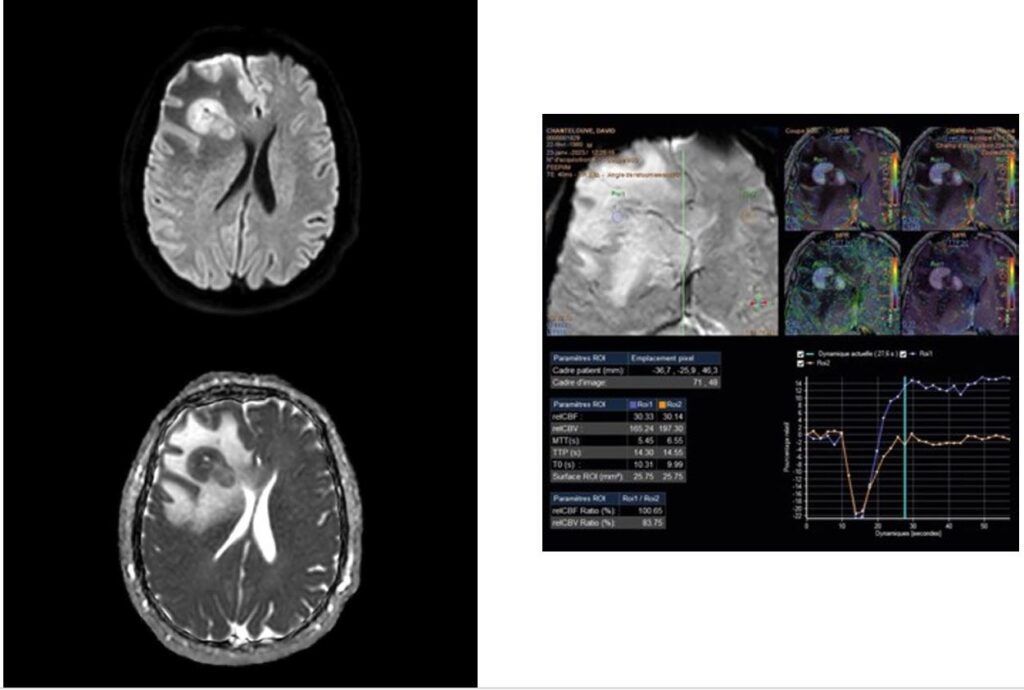
Fig. 2. Magnetic resonance imaging (MRI). A. Diffusion: right centrofrontal macrolobulated lesion (A). It presents a DWI [diffusion-weighted imaging] B1000 hypersignal with apparent diffusion coefficient (ADC) drop. B. Perfusion: cerebral blood volume
is not increased (165 on the lesion versus 197 in a healthy region) which is not in favor of an aggressive glial lesion. Significant rise in the curve after the first passage above the baseline: typical appearance of a blood-brain barrier rupture.
Fig. 3. Magnetic resonance spectroscopy. The spectroscopic profile of the lesion is represented by the yellow curve. A. On the short echo time (TE): lipid/lactate peak. B. On the long TE: N-acetyl aspartate (NAA) drop and choline peak.
CONCLUSION
The contribution of MRI and more particularly perfusion MRI and MRS seems obvious in the diagnosis of brain tumors and lymphoma specifically. In this case, the MRI report suggested a diagnosis of cerebral lymphoma, allowing physicians to prepare in advance to treat this potential affection.
Radiology is no longer limited to an anatomical study but allows a functional approach. The radiological data can have a sufficient specificity to make a biopsy obsolete.
In the meantime, with the arrival and the improvement of new radiological tools (such as the spectral computed tomography), radiologists will try to find the best anatomical and functional imaging markers in order to improve patient care.
REFERENCES
- Villano JL, Koshy M, Shaikh H, et al. Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer. 2011;105:1414-8.
- Batchelor TT. Primary central nervous system lymphoma: a curable disease. Hematol Oncol. 2019;37(S1):15-8.
- Cotton F, Ongolo-Zogo P, Louis-Tisserand G, et al. [Diffusion and perfusion MR imaging in cerebral lymphomas] [in French]. J Neuroradiol. 2006;33(4):220-8.
- Hartmann M, Heiland S, Harting I, et al. Distinguishing primary cerebral lymphoma from high-grade glioma with perfusion-weighted magnetic resonance imaging. Neurosci Lett. 2003;338(2):119-22.