INTRODUCTION
Headache is one of the most common complaints worldwide with a lifelong prevalence of 96% in the general population [1]. According to the 3rd edition of the International Classification of Headache Disorders (ICHD-3), all headache disorders are classified into two major groups: primary and secondary headaches [2]. The worldwide prevalence of secondary headaches is estimated at 18% [3]. Many headaches are benign and short-lasting, without the need for any treatment. However, every specialist, who deals with headaches, should be very careful, as headaches can be the primary and the only sign of a serious and sometimes even a life-threatening disease. The mnemonic SNOOP and the newer version SNNOOP10 including Systemic disease, Neoplasm in history, Neurological dysfunction, abrupt Onset, Old age, Positional nature of headache, Pregnancy and other features (Table 1) were proposed to easily detect red flags for secondary headaches [3]. “Pattern change or recent onset of new headache” is one of the red flags in SNNOOP10 list, and the prevalence of this phenomenon in headaches is not known [3]. From 8.2% to 40% of patients in different studies had headaches as the only symptom of a serious disorder (thrombosis, brain lesion or tumor). In these patients, the accurate diagnosis was delayed for 9±6.7 days [3]. Therefore, it is of ultimate importance to attempt to distinguish between the primary and secondary headaches at the initial visit of a new patient.
In this article, we report a case of cerebral venous sinus thrombosis (CVT) in association with previously undiagnosed hyperthyroidism and presenting with severe new-onset headache as the only symptom of CVT.
CASE REPORT
A 50-year-old, right-handed female presented to the outpatient department at “Vanadzor” Medical Center (Vanadzor, Armenia) with a history of three-day-long very severe headache with episodic nausea and a single episode of vomiting. She denied any severe headache or chronic disease prior to the current episode. The headache was unresponsive to non-steroidal anti-inflammatory drugs (NSAIDs). The neurological examination was normal, except that the patient appeared restless and exhausted. The patient refused the computed tomography (CT) scan due to financial difficulties. Ibuprofen 800-1200 mg was prescribed, and the patient chose to be discharged despite given advice.
Table 1. SNNOOP10 list of red and orange flags [3]
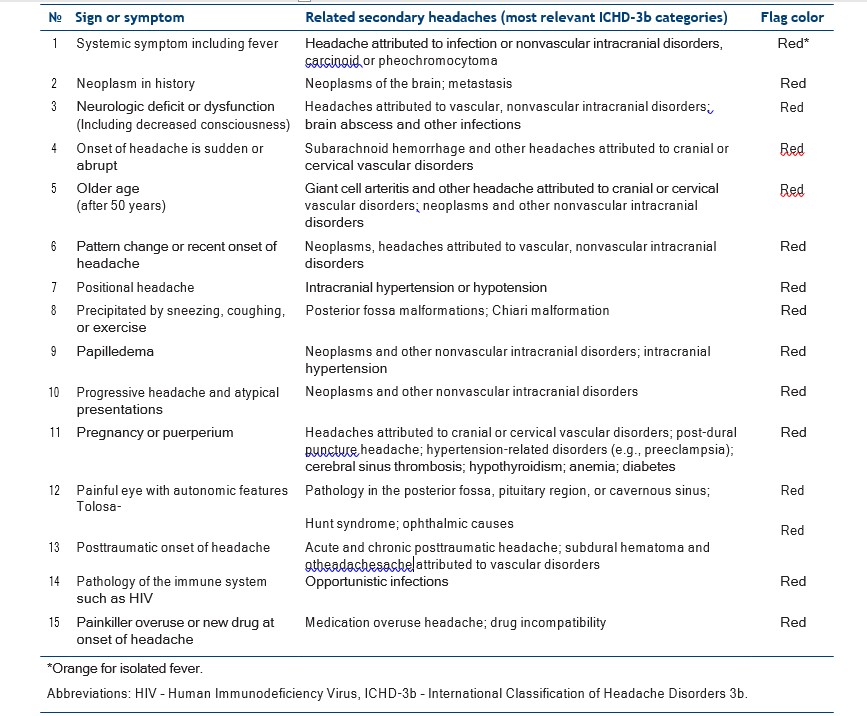
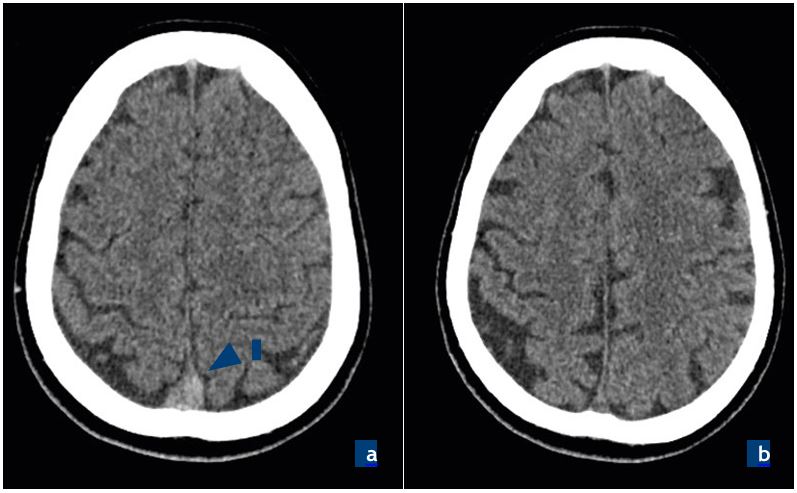
Figure 1. Computed tomography (CT) scans of the patient – axial view:
a. first CT, ‘‘dense triangle sign’’ (red arrow), b. follow-up scan (3-month after discharge).
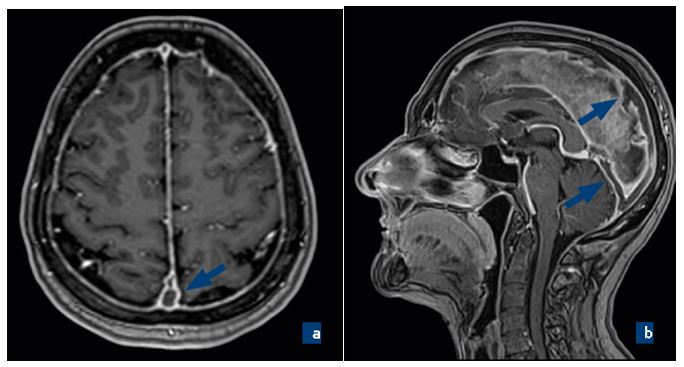
Figure 1. Contrast-enhanced magnetic resonance imaging (MRI) of the patient before treatment:
a. axial view, b. sagittal view. Thrombosis of superior sagittal and straight sinuses (arrows).
Two days later the patient was re-admitted to the emergency unit with the same complaints. She stated that the headache became worse during the last two days, at the morning of admission she had involuntary shaking movements in her right arm and its weakness. An urgent CT scan without contrast was performed which suggested a thrombosis of the superior sagittal, straight, and left transverse sinuses (Fig. 1a). The patient was referred to a specialized hospital for further evaluation and management.
Three hours later the patient was admitted to the neurological department at “Erebouni” Medical Center (Yerevan, Armenia). Upon examination, the patient was confused and disoriented. There were no other abnormalities on neurological examination. Magnetic resonance imaging (MRI) of the head (1.5T) with contrast enhancement (Fig. 2) and CT of paranasal sinuses were performed. MRI scan showed thrombosis of the superior sagittal, sigmoid, left transverse sinuses and proximal part of the left internal jugular vein, meningitis (diffuse accumulation of contrast in meninges), and inflammation of the right maxillary sinus. CT scan confirmed right-sided maxillary sinusitis. There were no signs and symptoms of infection and inflammatory processes (normal white blood cells and body temperature). Pathological laboratory findings revealed anemia (low hemoglobin 9.5 g/dL [normal range: 12-16], red blood cells 2.67×1012/L [normal range: 3.92 to 5.13], hematocrit 24.5% [normal range: 36-48]) and low level of thyroid stimulating hormone < 0.005 µIU/mL (normal range: 0.5-10). Other laboratory findings (rest of complete blood count, clinical urine tests, blood chemistry, prothrombin time, INR, CRP, ANA, Anti-ds-DNA, Anti-β2-Glycoprotein IgG/IgM, ANCA, tests for DNA polymorphisms in thrombosis-related genes FII and FV) were unremarkable. Antithrombotic therapy with enoxaparin 0.6 mg bid and warfarin 2.5 mg/day started immediately. Acetazolamide 500 mg/day and Levetiracetam 1000 mg/day was also prescribed. Six days later the patient was stable, with mild to moderate headaches. She was sent back to “Vanadzor” Medical Center for further treatment. Antithrombotic (warfarin 6.25 mg with INR control between 2-3), anticonvulsant (levetiracetam 1000 mg 250 mg, discontinued on day 7), antithyroid (thiamazole 10 mg qid) symptomatic and supportive therapy was performed. The patient was discharged 8 days later with mild headaches and no neurological deficit. Warfarin 6.25 mg, bisoprolol 2.5mg, thiamazole 10mg qid, and paracetamol 1000 mg
in cases of severe headaches were prescribed. At three-month follow-up, the patient had no complaints with no abnormalities on CT scan (Fig. 1b). Warfarin was discontinued 6 months after the initiation. Thiamazole was continued and monitored by an endocrinologist.
DISCUSSION
In patients with headache without any red flags present, imaging, and laboratory work-up are usually not indicated if the patient is evaluated thoroughly by a medical doctor who is aware of the red flags [4]. Thus, running a standard pack of studies, including imaging and blood tests, is not recommended in every patient, since the risk of false-positive results and incidental findings is high. In a prospective study with 3655 non-acute headache patients, only 14.5% of patients had red flags present leading to neuroimaging in which only 2.1% of scanned patients (0.3% of all participants) were found to have imaging abnormalities [5]. Similar results were found in other retrospective and prospective studies [3]. In 2003, the mnemonic SNOOP was suggested followed by SNNOOP10 in 2019 [3] (Table 1), meant to help physicians navigate in possible secondary headaches. The sensitivity of red flags is known; however, their specificity and predictive values are also necessary to investigate.
The probability of detecting a secondary headache is higher in emergency departments, where headache can be the primary and the only symptom [6]. In such circumstances, using red flags facilitates decision-making process easier for a physician. CVT is an uncommon cause of stroke. It can be caused by various conditions of hypercoagulable state (infections, autoimmune, traumatic, iatrogenic, etc.) [6]. Headache, focal neurologic deficit, mental status changes, and seizures are common signs of CVT [6]. Symptoms can be nonspecific, and a native CT scan can be non-informative. The diagnostic methods of choice are MRand CT-venography. The ‘‘dense triangle sign’’ (hyperdensity of the thrombosed sinus [Fig. 1a] can be found as the only sign in many cases on a non-contrast cerebral CT scan, which should not be missed [7].
Hyperthyroidism is a common condition with various signs and symptoms. Several studies suggested the role of hyperthyroidism in hypercoagulable states. Increased factor VIII was suggested as the main reason [8]. Thus, hyperthyroidism may be associated with cerebral venous thrombosis including the current patient. The association of CVT and hyperthyroidism was first described by Kaliebe in 1913 [9]. Almost 50 cases have been reported so far [10-15]. However, these cases are rare, and systematized studies have not been performed yet.
CONCLUSION
We describe a 50-year-old previously healthy female patient with a thrombosis of the superior sagittal, sigmoid, left transverse sinuses, and proximal part of the left internal jugular vein as a possible consequence of previously undiagnosed hyperthyroidism. On the initial examination the only symptom was severe, new-onset headache, which was not responsive to any NSAIDs. The use of red flags from the SNNOOP10 list helped to make a correct diagnosis and initiate appropriate treatment as soon as possible.
REFERENCES
- Rizzoli P, Mullally WJ. Headache. Am J Med. 2018;131(1):1724.
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211.
- Do TP, Remmers A, Schytz HW, et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology. 2019;92(3):134-144.
- García-Azorín D, Abelaira-Freire J, González-García N, et al. Sensitivity of the SNNOOP10 list in the high-risk secondary headache detection. Cephalalgia. 2022;42(14):15211531.
- Clarke CE, Edwards J, Nicholl DJ, Sivaguru A. Imaging results in a consecutive series of 530 new patients in the Birmingham Headache Service. J Neurol. 2010;257(8):12741278.
- Dodick D. Headache as a symptom of ominous disease: What are the warning signals? Postgraduate Medicine. 1997;101(5):46-64.
- Timóteo Â, Inácio N, Machado S, Pinto AA, Parreira
E. Headache as the sole presentation of cerebral venous thrombosis: a prospective study. J Headache Pain. 2012;13(6):487-490. - Mouton S, Nighoghossian N, Berruyer M, et al. Hyperthyroidism and Cerebral Venous Thrombosis. Eur Neurol. 2005;54(2):78-80.
- Son HM. Massive cerebral venous sinus thrombosis secondary to Graves’ disease. Yeungnam Univ J Med. 2019;36(3):273-280.
- Franchini M, Lippi G, Targher G. Hyperthyroidism and venous thrombosis: a casual or causal association? A systematic literature review. Clin Appl Thromb Hemost. 2011;17(4):387-392.
- Merino M, Guijarro MG, Iglesias P, Aladro Y, Montero P. Tirotoxicosis y trombosis de senos venosos cerebrales, ¿causalidad o azar? [Thyrotoxicosis and cerebral venous sinus thrombosis, causality or chance alone?]. Endocrinol Nutr. 2012;59(7):462-463.
- Migeot M, Rutgers MP, Gille M. Puerperal cerebral sinus venous thrombosis and acute hyperthyroidism in Graves’ disease. Acta Neurol Belg. 2013;113(3):331-333.
- Rivoisy C, Desforges V, Tir M, et al. Thrombophlébite cérébrale : penser à l’hyperthyroïdie. Revue Neurologique. 2010;166(4):467-469.
- Hwang JU, Kwon KY, Hur JW, Lee JW, Lee HK. The Role of Hyperthyroidism as the Predisposing Factor for Superior Sagittal Sinus Thrombosis. J Cerebrovasc Endovasc Neurosurg. 2012;14(3):251.
- Hermans E, Mariën P, De Deyn PP. Sinus sigmoideus thrombosis secondary to Graves’ disease: a case description. Case Rep Neurol. 2011;3(3):203-209.