Всеобъемлющий систематический обзор гистеросальпингоконтрастной сонографии (HyFoSy) и гистеросальпингопеной сонографии (HyFoSy)
Костас Панайотидис
Центр передовой гинекологической ультразвуковой диагностики и гистероскопии Attiki Iatriki, Греция
Абстракт
Гистеросальпингоконтрастная сонография (HyCoSy) и гистеросальпингопеная сонография (HyFoSy) — это современные, минимально инвазивные методы, используемые для оценки проходимости маточных труб, что является важным аспектом при обследовании женского бесплодия. Данный систематический обзор направлен на всесторонний анализ этих методик, включая их принципы, детали проведения, эффективность, безопасность и сравнение с традиционными методами, такими как гистеросальпингография (HSG). В обзоре обобщены результаты недавних исследований, клинических испытаний и мета-анализов с целью предоставить информацию о преимуществах, ограничениях и клиническом применении HyCoSy и HyFoSy, с особым акцентом на анализ затрат и экономические последствия.
DOI 10.54235/27382737-2024.v4.2-47
Introduction
Infertility affects approximately 10-15% of couples worldwide, with tubal factors accounting for a significant proportion of female infertility cases [1]. Assessing tubal patency is a critical step in infertility investigations. Traditional methods such as hysterosalpingography (HSG) and laparoscopy with chromopertubation, though effective, have limitations including invasiveness, radiation exposure, and patient discomfort [2]. HyCoSy and HyFoSy have emerged as alternatives, offering real-time, radiation-free, and less invasive options [3, 4]. This review systematically examines the available literature on HyCoSy and HyFoSy, focusing on their diagnostic accuracy, safety profiles, patient tolerability, cost-effectiveness, and comparative effectiveness.
Methodology
A systematic search was conducted in databases including PubMed, Embase, and Cochrane Library for studies published between January 1998 and June 2024. Keywords included “HyCoSy,” “HyFoSy,” “fallopian tube patency,” “infertility,” “contrast sonography,” “foam sonography,” “3D HyCoSy,” “3D HyFoSy,” and “cost analysis.” Inclusion criteria were peer-reviewed articles, clinical trials, meta-analyses, and systematic reviews focusing on the diagnostic use of HyCoSy and HyFoSy. Studies were excluded if they were not available in English, were case reports, or did not focus primarily on tubal patency assessment.
Principles of HyCoSy and HyFoSy
HyCoSy involves the transvaginal ultrasound-guided introduction of a contrast medium (usually an ultrasound contrast agent like Echovist® or saline with microbubbles) into the uterine cavity and fallopian tubes. The movement of the contrast medium through the tubes is observed in real-time using ultrasound, allowing for the assessment of tubal patency [5].
HyFoSy, on the other hand, uses a gel-based or foam contrast medium such as ExEm® Foam. The foam is instilled into the uterine cavity and observed as it travels through the fallopian tubes using ultrasound, see Figure 1.
The use of foam enhances the visibility as contrast medium, potentially improving diagnostic accuracy and patient comfort [6].
3D Imaging in HyCoSy and HyFoSy
The integration of three-dimensional (3D) imaging technology in HyCoSy and HyFoSy procedures has shown promise in enhancing the accuracy and diagnostic capabilities of these techniques, see Figure 2.
- Enhanced Visualization: 3D imaging provides a more comprehensive view of the uterine cavity and fallopian tubes, allowing for better spatial resolution and more detailed assessment of tubal patency and uterine anomalies [7].
- Improved Accuracy: Studies have indicated that 3D HyCoSy and 3D HyFoSy can improve diagnostic accuracy compared to 2D imaging. For example, Alcázar et al. demonstrated that 3D power Doppler HyCoSy significantly improved the visualization of tubal patency and identified peritubal adhesions more accurately than 2D HyCoSy [8].
- Quantitative Analysis: 3D imaging allows for quantitative analysis of the uterine and tubal structures, which can be useful in planning treatment strategies and monitoring therapeutic outcomes [9].
Contrast Media: Types and Analysis
HyCoSy Contrast Media
- Echovist® (Levovist):
- Composition: Contains galactose and palmitic acid, forming microbubbles when mixed with water.
- Advantages: Good echogenicity, widely studied.
- Limitations: Potential for allergic reactions, discomfort during the procedure. These contrast media are not licensed for use in gynaecological invasive ultrasound techniques.
- Studies: Exacoustos et al. demonstrated that Echovist® provides clear visualization of tubal patency with high diagnostic accuracy [10].
- Author Experienced Opinion: Echovist® is reliable and provides consistent results, although some patients may experience transient discomfort during the procedure mainly because higher volume of medium is necessary to be used.
- Saline with Microbubbles:
- Composition: Saline solution mixed with air to create microbubbles.
- Advantages: Inexpensive, readily available, minimal risk of allergic reactions.
- Limitations: Short-lived echogenicity, requiring rapid imaging.
- Studies: Klangsin et al. found saline with microbubbles to be effective for tubal patency assessment, with comparable accuracy to HSG [11].
- Author Experienced Opinion: Saline with microbubbles is cost-effective and easy to prepare, but the imaging window is shorter, necessitating swift execution by the sonographer.
HyFoSy Contrast Media
- ExEm® Foam:
- Composition: A gel-based medium combined with air to create a foam. It is licensed for use in intrauterine cavity as contrast medium.
- Advantages: Enhanced visibility, better adherence to tubal walls, less discomfort.
- Limitations: Slightly more expensive than saline, rare cases of allergic reactions.
- Studies: Ludwin et al. reported high sensitivity and specificity for ExEm® Foam, making it a preferred choice in many clinical settings [12].
- Experienced author Opinion: ExEm® Foam is particularly effective for difficult cases where detailed visualization is essential. Its ability to provide sustained visibility makes it highly useful in clinical practice.
Efficacy and Diagnostic Accuracy
Several studies have evaluated the efficacy and diagnostic accuracy of HyCoSy and HyFoSy compared to traditional methods. Key findings include:
- Sensitivity and Specificity: Both HyCoSy and HyFoSy demonstrate high sensitivity and specificity in detecting tubal patency, often comparable to HSG and laparoscopy. A meta-analysis by Dreyer et al[13] reported a pooled sensitivity and specificity of HyCoSy compared with laparoscopy with chromopertubation of 0.92 (95% CI, 0.87–0.95) and of 0.89 (95% CI, 0.83–0.93), respectively. The pooled sensitivity and specificity of HyCoSy compared with HSG were 0.94 (95% CI, 0.88–0.97) and 0.91 (95% CI, 0.87–0.95), respectively. using Echovist®].
The sensitivity and specificity of hysterosalpingo-foam sonography compared with laparoscopy were 0.75 (95% CI 0.71 to 0.79) and 0.70 (95% CI 0.65 to 0.74) respectively [14]. The sensitivity of HyFoSy for detecting tubal patency was 76.3% with a specificity of 40%. The positive and negative predictive values were 82.9% and 30.8% respectively [15] A comparison of hysterosalpingo-foam sonography (HyFoSy) and hysterosalpingo-contrast sonography with saline medium (HyCoSy) in the assessment of tubal patency [16] showed higher proportion of patients in the HyCoSy group required crossover testing for verification of the findings. Whether HyFoSy is as accurate as HSG in evaluating tubal patency was studied by van Rijswijk J et al , [17] and concluded that HyFoSy and HSG have a concordance of 85%.
While both techniques are effective, some studies suggest that HyFoSy may provide superior visualization due to the properties of the foam contrast medium. The foam’s ability to adhere to the tubal walls and produce clear, sustained images can enhance diagnostic accuracy. This is because the microbubbles within the foam tend to coalesce and stabilize quickly, preventing the formation of larger bubbles compared to those created in normal saline. The high echogenicity of air and the characteristic flow of microbubbles in Exem® foam make the movement easily distinguishable, even for less experienced gynecologists, avoiding confusion with natural bubble movements often seen in the adjacent intestines near the uterine cornua and fallopian tubes.
However, experienced sonographers can identify the microbubble flow within normal saline with practice, as their ability to recognize specific image patterns improves over time. This is why HyCoSy is considered operator-dependent for tubal screening. The sonographic signal created with Exem® foam is more uniform and last longer, allowing both tubes to be studied and compared effectively. In contrast, when using normal saline and microbubbles for HYCOSY, the bubbles need to be regenerated to achieve a similar flow, which can be challenging when studying the second tube and comparing findings. To address this, specialized devices like FemVue® [18] have been developed, which can provide a constant flow with a consistent amount of microbubbles injected into the uterine cavity .
- Comparison with HSG: Studies indicate that HyCoSy and HyFoSy offer similar diagnostic accuracy to HSG but with the added benefits of no radiation exposure and better patient tolerance. For example, Ludwin et al. found that HyFoSy had a sensitivity of 94.2% and a specificity of 89.3% compared to HSG [19].
- Real-time Visualization: One of the significant advantages of HyCoSy and HyFoSy is the ability to provide real-time visualization of tubal patency, allowing immediate assessment and reducing the need for follow-up procedures [20].
- Impact of 3D Imaging: The use of 3D imaging further enhances these benefits. Ludwin et al. highlighted that 3D HyFoSy provided clearer and more detailed images compared to 2D imaging, improving the overall diagnostic process [6, 8,9,21,22.].
- Author Experienced Opinion: In clinical practice, the real-time feedback and immediate results provided by HyCoSy and HyFoSy significantly enhance the patient experience and allow for prompt decision-making regarding further fertility treatments.
Safety and Patient Tolerability
- Safety: Both procedures are generally safe, with minimal risk of complications. The most common adverse effects reported include mild discomfort, transient pain, and minor vaginal bleeding. Serious complications such as infection or allergic reactions to the contrast medium are rare [23,24].
- Patient Tolerability: Studies consistently report higher patient tolerability for HyCoSy and HyFoSy compared to HSG. The absence of radiation [25] , the minimally invasive nature, and the use of ultrasound contribute to a more comfortable experience.
A patient satisfaction survey by Saunders et al. indicated that 85% of patients preferred HyFoSy over HSG [16, 26].
- Author Experienced Opinion: often report less anxiety and discomfort with HyCoSy and HyFoSy compared to HSG, making these procedures more acceptable and easier to perform in an outpatient setting.
Clinical Outcomes
Recent studies have investigated the impact of HYCOSY and HYFOSY techniques on clinical outcomes including spontaneous pregnancy rates after the tests. Hardel et al. [27] compared pregnancy rates following intrauterine insemination (IUI) after HyFoSy and HSG, finding no significant difference in pregnancy rates but suggesting that HyFoSy might offer a quicker time to pregnancy due to more comprehensive and rapid management. Bisogni et al [28] using advanced ultrasound technique of
4D transvaginal scan and HYCOSY reported 30% of spontaneous pregnancy for young healthy women ( 358 patients) with bilateral or unilateral tubal patency of 30% within 2 months after the HYCOSY. Van Schoubroeck et al. studied 359 women post HyFoSy; 81 conceived spontaneously, with the majority of conceptions occurring within the first one to three menstrual cycles [29].
The author gives a comprehensive etiology why after HSG or HYFOSY / HYCOSY we observe following the tests after 1 to 2 months higher rates of spontaneous pregnancies. In all so far published reports, no one has commented about the existence of a dominant follicle during the HYCOSY or HYFOSY test, the dominant follicle measurements, and which day of the menstrual the test was performed. The test of HyCoSy / HyFoSy usually is done the eighth, ninth or tenth day of the menstrual but it can be done in pre and post ovulatory phase of the cycle. In other words, for women that HyCoSy or HyFoSy show bilateral tubal passage some patients may undertake intercourse in the next days but some not, however, if the gynecologist who performed the test, calculate the potential day of ovulation and indicate this encouraging the patience to have intercourse then the chances for spontaneous conception are raised. So it may not be the technique as such that increase the fertility but the fact that for some couples, their intercourses are best synchronized with ovulation knowing that the tubes likely are patent. This observation is based on unpublished data of the author and the success rate for the next 2-3 months is about 15-20 %. The calculation of the increased size of the dominant follicle is based on 1-1.5 mm growth per day -mean diameter of the dominant follicle. The practice to calculate in a normal cycle, the day of ovulation using ultrasound is not commonly performed and most of the fertility services would like to know about the condition of the fallopian tubes without enhancing the synchronization of intercourse, taking advantage of this technique.
Cost Analysis
The cost of HyCoSy and HyFoSy procedures is influenced by several factors, including the price of contrast media, the intrauterine or intracervical catheter, and the overall procedural costs.
- Contrast Media Costs: The cost of Echovist® and ExEm® Foam can be significantly higher than saline with microbubbles. For instance, ExEm® Foam costs approximately $150-200 per procedure, whereas saline with microbubbles can cost as little as $10-20 [30, 31].
- HYCOSY – HYFOSY Catheter Costs: The specialized catheters used in these procedures can add to the overall cost. Single-use catheters typically range from $30-50 each [32]. It is important to note that there are two types of catheters used:
- the exocervical see Figures 3 and 4
- the intracervical or intrauterine catheter see
Figures 5 and 6
The exocervical has a conical end, which is used like a cork to obstruct the cervix avoiding reflux of the contact medium / or saline. The intracervical or intrauterine catheter are double lumen catheters having a inflatable balloon in order obstruct the inner part of the cervix or to be positioned at the level of uterine isthmus. The amount of fluid needed for bilateral passage of the contrast medium depends as well on the type of catheter which is used for this procedure; the ones that they are exocervical may need couple of milliliters more fluid in order to increase the intrauterine in pressure in a such level to allow bilateral passage. In the contrary using intrauterine catheters positioned higher up the amount of fluid needed for bilateral visualization is much less. Overall, 4 ml of medium should be (under good conditions and if the uterus is completely normal in shape) enough to demonstrate bilateral passage. This is a fact that should be taking into consideration when expensive contrast mediums are used.
- Total Procedure Costs: When considering the total procedure costs, including sonographer fees, radiologist fees, and facility charges, the average cost of HyCoSy or HyFoSy ranges from $300-600 per procedure [33]. In Europe a HSG is valued for about 150-200 Euros (where reusable instruments are used), expert ulstrasonographer who combine advanced gynecological ultrasound assessment and medium injection for HYFOSY or HYCOSY may charge 180-250 euros. Some if only the HYCOSY is done commenting only about the tubal patency without completing a full gynaecological ultrasound assessment may charge as much as for HSG meaning 150 Euros.
- Cost-Effectiveness: Despite the higher initial costs, HyCoSy and HyFoSy can be more cost-effective in the long run. The real-time results, reduced need for additional imaging, and lower risk of complications can offset the higher costs of contrast media and specialized catheters. A cost-effectiveness analysis by Maheshwari et al. concluded that HyFoSy was more cost-effective than HSG when considering the overall patient journey and associated costs [30, 31].
As well consideration should be given for the cost those doctors who practice in a sequential way regarding the ultrasound assessment, meaning some offer a first visit with endovaginal assessment and after this a secondary visit for HYCOSY or HYFOSY. The cost should add the cost of these 2 separate examinations which overpass the 250+300 euros. In other words best cost effectiveness is to be expected when we combine gynaecological scan (complete assessment for fertility ) and then during the same examination session to proceed with contrast medium injection for the assessment of the tubes in one appointment.
- Author Experienced Opinion: While the initial costs of HyCoSy and HyFoSy might be higher, the long-term benefits and potential savings from reduced follow-up procedures make them a cost-effective choice for many clinics essentially for those women who appear to have normal uterus and tubes. Importance should be given on how to manage cases where the HyCoSy- HyFoSy suggest obstruction (uni or bilateral). it is concerning that some practices do not proceed with the diagnostic (and some times therapeutic when surgery can be done ) laparoscopy and proceed directly to IVF-ICSI techniques. In these cases, the accuracy of the ultrasonographer is not evaluated with the danger to overestimated false pathological findings.
Discussion and Future
Research developments
HyCoSy and HyFoSy represent significant advancements in the field of reproductive medicine, offering safe, effective, and patient-friendly alternatives for assessing tubal patency. The integration of 3D imaging technology further enhances the diagnostic capabilities of these procedures, making them valuable tools in infertility investigations. The choice of contrast media, procedural techniques, and the expertise of the operator are crucial factors influencing the success and diagnostic accuracy of HyCoSy and HyFoSy. Ongoing research and technological advancements are expected to further improve these techniques, making them even more accessible and cost-effective.
Future research should focus on long-term outcomes of patients diagnosed using HyCoSy and HyFoSy, comparative studies to refine protocols, and technological advancements to further improve diagnostic accuracy and patient experience. Additionally, studies exploring the integration of these techniques into broader infertility treatment pathways will be valuable. Emerging contrast agents and improvements in ultrasound technology also hold promise for enhancing the effectiveness of these procedures.
Appropriate training is another issue for the future research. A difficult question to answer is about who should perform HYCOSY or HYFOSY? and what training level or ultrasound capacity should be achieved before the operator is practicing these techniques. There are 3 levels of ultrasound capacity as described by the European federation of societies for ultrasound in Medicine [34]. Regarding the gynaecological ultrasound Level 1 corresponds to basic level where the operator is able to recognize normal anatomy, for level 2 the operator acquires the capacity to recognize and describe common pathologies and level 3 correspond to an expert level where advanced ultrasound techniques are routinely used. However, there is no guideline or standards described so far about who can perform HYCOSY or HYFOSY. HyCoSy and HyFoSy is one of the four invasive ultrasound guided techniques (the other three are the Oocyte Pick UP, the Embryo transfer, the transvaginal cyst aspiration).
The author suggests that the HYFOSY or HYCOSY for tubal patency exploration should be undertaken by ulstrasonographer or gynecologist with at least level 2 experience and from those that are trained in 3D gynaecological imaging. Although these techniques are used more than 10-15 years few reported what is the real accuracy of the tests in current practice and what should be the “acceptable” rate of false positives or negatives tolerated outside the research studies set up. Due to the commercial interests promoting patient friendly techniques, more and more gynecologists undertake these services without having competed a scrutinized training and after a short period of learning (mainly on how to introduce the catheter) start to provide services on tubal patency with ultrasound assessment. A guideline and standards of practice for these new techniques is mandatory for accurate and safe use of HYCOSY and HYFOSY.
Conclusion
HyCoSy and HyFoSy are valuable diagnostic tools for assessing tubal patency, offering significant advantages over traditional methods such as HSG. Their high diagnostic accuracy, safety, patient tolerability, and cost-effectiveness make them preferable choices in modern infertility investigations. The integration of 3D imaging technology further enhances their diagnostic capabilities, providing detailed and accurate assessments of tubal patency and uterine anomalies. Continued research and technological advancements will likely further improve these techniques, making them indispensable in the field of reproductive medicine.
References
- Evers JL. Female subfertility. Lancet. 2002;360(9327):151-159.
- Steinkeler JA, Woodfield CA, Lazarus E, Hillstrom MM. Female infertility: a systematic approach to radiologic imaging and diagnosis. Radiographics. 2009;29(5):1353-1370.
- Exacoustos C, et al. Contrast-tuned imaging and Doppler ultrasound in the assessment of tubal patency. AJR Am J Roentgenol. 2007;189(6):1300-1305.
- Saunders RD, et al. Hysterosalpingo-foam sonography (HyFoSy): a new technique for tubal patency testing. Hum Reprod. 2012;27(3):715-720.
- Emanuel MH, et al. A prospective comparative study of chlamydia antibody testing, hysterosalpingography, and hysterosalpingo-contrast sonography in subfertile women. Fertil Steril. 1998;70(5):948-955.
- Ludwin A, et al. Three-dimensional hysterosalpingo-foam sonography (3D-HyFoSy) with ExEm® Foam for the evaluation of fallopian tube patency. Ultrasound Obstet Gynecol. 2017;50(2):245-247.
- Alcázar, J L et al. Two-dimensional hysterosalpingo-contrast-sonography compared to three/four-dimensional hysterosalpingo-contrast-sonography for the assessment of tubal occlusion in women with infertility/subfertility: a systematic review with meta-analysis. Human Fertility 2020;25(1), 43–55.
- Alcázar JL, et al. Three-dimensional power Doppler hysterosalpingo-contrast sonography for the assessment of tubal patency and peritubal adhesions. J Ultrasound Med. 2009;28(12):1559-1564
- JFA KW, et al. Comparative effectiveness of 3D imaging in hysterosalpingo-contrast-sonography versus conventional methods for evaluating tubal patency. Fertil Steril. 2021;115(4):891-900
- Exacoustos, R., et al. Hysterosalpingo-contrast-sonography with Echovist for the assessment of tubal patency: a comparison with laparoscopy and hysterosalpingography. Hum Reprod. 2009;24(3):606-12.
- Klangsin, S., et al. Hysterosalpingo-Foam Sonography for Tubal Patency Testing: Comparison with Hysterosalpingography and Laparoscopy. Ultrasound Obstet Gynecol. 2018;51(5):668-74
- Ludwin, A., et al. Hysterosalpingo-Foam Sonography (HyFoSy) with ExEm® Foam for Tubal Patency Testing: A Comparative Study. Hum Reprod. 2016;31(4):809-17.
- Dreyer K, et al. Hysterosalpingo-contrast-sonography (HyCoSy) in the diagnosis of tubal patency: a systematic review and meta-analysis. Ultrasound Med Biol. 2019;45(7):1392-1402
- Le MT, et al. Diagnostic accuracy of hysterosalpingo-foam sonography for assessment of fallopian tube patency in infertile women. Reprod Biomed Online. 2024 May 16;49(3):104112
- Dordoni D, et al. Comparison of hysterosalpingo-foam-sonohysterography (HyFoSy) with laparoscopic chromosalpingography in the assessment of tubal patency in infertile patients. Fertil Steril. 2013 Sep;100(3 Suppl)
- Lim SL, Jung JJ, Yu SL, Rajesh H. A comparison of hysterosalpingo-foam sonography (HyFoSy) and hysterosalpingo-contrast sonography with saline medium (HyCoSy) in the assessment of tubal patency. Eur J Obstet Gynecol Reprod Biol. 2015 Dec;195:168-72
- van Rijswijk J, van Welie N, Dreyer K, et al. The FOAM study: is hysterosalpingo foam sonography (HyFoSy) a cost-effective alternative for hysterosalpingography (HSG) in assessing tubal patency in subfertile women? Study protocol for a randomized controlled trial. BMC Womens Health. 2018;18(1):64.
- Smith AD, Smith RD, Bhattacharya S. FemVue device in hysterosalpingo-contrast sonography (HyCoSy): An evaluation of diagnostic effectiveness. J Obstet Gynaecol Res. 2022;48(4):789-795.
- Ludwin I, et al. Accuracy of hysterosalpingo-foam sonography (HyFoSy) in comparison to hysterosalpingography (HSG) in the assessment of tubal patency: A prospective, randomized study. Ultrasound Obstet Gynecol. 2017;49(1):104-110.
- Reuter K, Witzenbichler C, Fiebelkorn T, et al. Comparison of Hysterosalpingo-Contrast Sonography (HyCoSy) and Hysterosalpingography (HSG) for Tubal Patency Assessment: A Prospective Study. Ultrasound Obstet Gynecol. 2017;49(3):377-382.
- Exacoustos C, Di Giovanni A, Szabolcs B, Binder-Reisinger H, Gabardi C, Arduini D. Automated three-dimensional hysterosalpingo-contrast sonography: feasibility of a novel technique for evaluation of tubal patency. J Ultrasound Med. 2013;32(5):827-834
- Sallam HN, Agameya AF, Rahman AF, Ezzeldin F. Three-dimensional (3D) ultrasound as a diagnostic tool for tubal patency assessment in infertility patients: a comparison with hysterosalpingography. Middle East Fertil Soc J. 2003;8(3):227-232
- Kamel RM, El-Din AB, Elnashar A, et al. Hysterosalpingo-Contrast Sonography Versus Hysterosalpingography for Evaluating Fallopian Tube Patency: A Systematic Review. Fertil Steril. 2018;109(1):115-122
- Engels V, Medina M, Antolín E, Ros C, Amaro A, De-Guirior C, Manzour N, Sotillo L, De la Cuesta R, Rodríguez R, San-Frutos L, Peralta S, Martin-Martínez A, Alcázar JL. Feasibility, tolerability, and safety of hysterosalpingo-foam sonography (HyFoSy). J Gynecol Obstet Hum Reprod. 2021;50(5):102004.
- langsin S, Matemanosak P, Peeyananjarassri K, Wattanakumtornkul S, Tubtawee T, Trongnit S, Geater AF. Effect of radiation on serum anti-Müllerian hormone during hysterosalpingography in female infertility. Reproductive BioMedicine Online. 2024;48(6):103843.
- Tsiami A, Hill J, Shakeri N, et al. Patient Tolerability and Diagnostic Performance of Hysterosalpingo-Foam Sonography. Reprod Biol Endocrinol. 2022;20(1):123.
- Hardel A, Tran P, Flye Sainte Marie H, Boukerrou M. Grossesse après hystérosalpingo-Foam-Sonographie. Gynécologie Obstétrique Fertilité & Sénologie. 2024;52(5):375-376.
- Bisogni FA, Galanti F, Riccio S, et al. 4D-HyCoSy performed in a reproductive center: retrospective analysis of pain perception, complications and spontaneous pregnancy rate after the technique. Eur Rev Med Pharmacol Sci. 2021;25:7468–7475
- Van Schoubroeck D, den Bosch TV, Van Tornout K, D’Hooghe T, Timmerman D. Spontaneous conception after hysterosalpingo-foam sonography (HyFoSy). Ultrasound Obstet Gynecol. 2015;46:51.
- Maheshwari A, Fluker M, Afnan M, et al. Economic Evaluation of Hysterosalpingo-Foam Sonography in Subfertility Treatment. Hum Reprod. 2021;36(5):1234-1242
- Maheshwari A, et al. Cost-effectiveness of Hysterosalpingo-Foam Sonography (HyFoSy) for tubal patency testing in subfertile women. Hum Reprod. 2020;35(4):839-845.
- Watanabe H, Kagawa N, Takeuchi H, et al. Cost Analysis of Different Contrast Media in HyCoSy. J Obstet Gynaecol Res. 2020;46(3):450-458.
- Khamis R, Islam R, Jansen A, et al. Economic Impact of Hysterosalpingo-Contrast Sonography: A Comparative Study. Fertil Steril. 2023;120(6):987-995.20. Maeda N, Takahashi K, Yoshida K, et al. Long-Term Cost-Effectiveness of HyFoSy in Infertility Diagnosis. J Reprod Med. 2022;67(1):45-53.
- European Federation of Societies for Ultrasound in Medicine and Biology https://efsumb.org/minimum-training-recommendations/, publications and guidelines, minimum training recommendation, appendix 3 (2009-04-14apx3) 2024, latest checked on 31/8/2024.
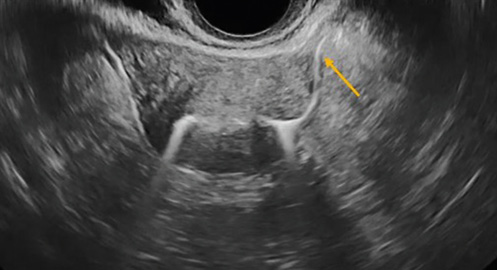
Figure 1. illustration of HYFOSY bilateral passage of ExEm® Foam, in this snapshot the passage from the left tube is seen clearly see yellow arrow
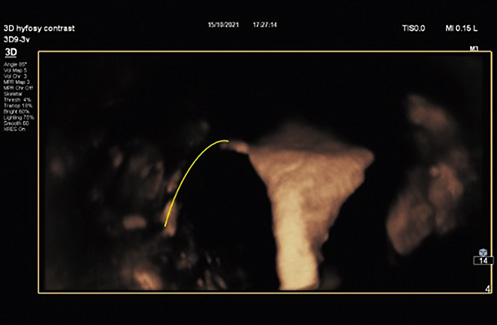
Figure 2. 3D HyFoSY study , the uterus is seen from its posterior view , the left tube is seen with partial passage of the foam, yellow line
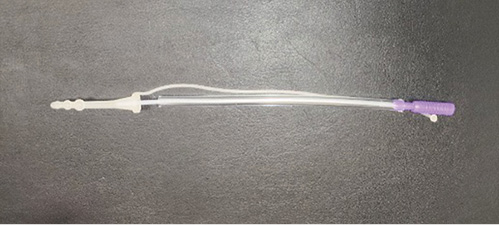
Figure 3. An example of an Exocervical catheter
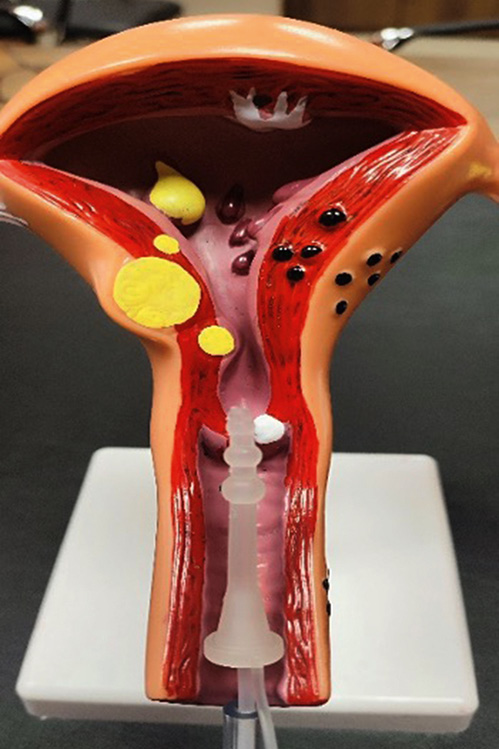
Figure 4. During the demonstration on a uterine model, the distal tip of the catheter is securely positioned on the exocervix. This placement helps prevent any potential reflux of the medium during the injection

Figure 5. intracervical / intrauterine double lumen catheter for HSG, HYCOSY and HYFOSY.

Figure 6. During the demonstration on a uterine model, the catheter is positioned within the upper part of the cervical isthmus. The catheter is secured by inflating a small balloon, which effectively blocks the upper part of the cervix