Каридакис против марсупиализации – краткосрочные сравнительные исходы лечения межъягодичной пилонидальной болезни у мужчин
Арман Мурадян 1, Арман Акобян 2, Эдгар Мартиросян 3, Гамлет Горхмазян 1, Ваган Геворкян 1, Ваагн Амбарцумян 1,4
1 Центральный клинический военный госпиталь, Отделение общей хирургии, Ереван, Армения
2 Факультет военной медицины, Ереванский государственный медицинский университет имени Гераци (ЕГМУ), Ереван, Армения
3 Кафедра военномедицинской хирургии, ЕГМУ, Ереван, Армения
4 Кафедра общей хирургии, ЕГМУ, Ереван, Армения
АБСТРАКТ
Цель: Настоящее исследование было направлено на заполнение пробела в знаниях о превосходстве доступных хирургических методов, используемых при лечении межъягодичной пилонидальной болезни (МПБ).
Методы: Ретроспективно сравнивали ближайшие исходы двух методов хирургического лечения МПБ, а именно процедуры Каридакиса (n = 32) и техники марсупиализации (n = 33). Изучали продолжительность полного формирования рубца, частоту развития краткосрочных послеоперационных осложнений, сохранение послеоперационной боли и частоту рецидивов в течение 3-месячного послеоперационного периода. Исследование было основано на ретроспективном анализе данных, извлечённых из медицинских карт взрослых пациентов мужского пола, проходивших лечение по поводу МПБ.
Результаты: Установлено, что процедура Каридакиса превосходит все вышеперечисленные параметры, за исключением частоты краткосрочных послеоперационных осложнений, где обе хирургические методики показали сопоставимые результаты.
Выводы: Результаты данного ретроспективного исследования позволяют предположить, что техника марсупиализации в хирургической практике может быть практически заменена операцией Каридакиса. Последнее, по-видимому, связано с более быстрым возвращением к повседневной деятельности и с большей экономической эффективностью.
Ключевые слова: межъягодичная пилонидальная болезнь, МПБ, марсупиализация, Каридакис.
DOI: 10.54235/27382737-2023.v3.1-42
Background
Intergluteal pilonidal disease (IPD) is a common chronic disease occurring in the natal cleft of the sacrococcygeal region, and it is more common among young males. Generally, male persons are 2 to 4 times more prone to this disease [1-3].
The main incidence ranges from 25/100,000 up to 48/100,000 in different populations [2,4,5]. The risk factors for IPD include obesity, local trauma or irritation, prolonged sitting, a deep natal cleft, and positive family history [1]. Although a wide range of surgical treatments has been used to manage IPD, none of these approaches eliminates the postoperative morbidity, including delayed wound healing, discomfort, and a high rate of recurrence, which differs in a wide range between 1% and 43% according to different studies [6-9]. Literature data suggest that recurrence is more related to the surgical procedure itself, and also correlates with the duration of follow up [3,5,10]. Along with the recurrence rates, the length of hospital stay, return to daily activities, and the cost-effectiveness of the treatment are also important when choosing a treatment method.
The most commonly used surgical techniques for IPD are wide excision followed by open wound healing; pit excision and tract brushing (Millar-Lord procedure); Bascom procedure; excision and marsupialization or suturing wound edges to bottom; excision and primary closure with midline or asymmetric incisions; or excision and closure using local flaps [11,12]. Each of the listed methods has its advantages and disadvantages, and the literature does not provide definitive guidance on the best method of surgical treatment. Management of the resultant defect in the tense sacral region appears to be the most challenging issue in the surgical treatment of IPD because this step is closely related to postoperative morbidity and recurrence [13].
Open wound healing after total excision is shown to have fewer early postoperative wound complications and relatively fewer cases of recurrence, but a relatively long duration of treatment. That is why many authors do not use this method routinely as a first-line treatment for IPD [14-16]. Primary wound closure after excision is associated with shorter healing time and hospital stay, but a high rate of recurrence and postoperative wound complications, according to many authors [17,18]. Our own experience also suggests not using this method widely.
Different recurrence rates (7% – 31.8%) have been published in cases of wound edges suturing to the wound floor after total excision of pilonidal tracts [16,19]. Perhaps the wide-ranging difference in recurrence rates was due to differences in postoperative care and research methodology.
Due to the low incidence of postoperative wound-related complications and the simplicity of the surgical technique, the surgical practice of suturing the skin flaps to the wound crater after total excision of pilonidal tracts has been widely used for a long time in our hospital.
Currently, the most popular surgical techniques are based on asymmetric wound closure (Karydakis or Bascom’s technique) or skin flap formation (Limberg, W- or Z-plasty). A theoretical option aiming to improve surgical outcomes and reduce the median recurrence rate involves the lateralization and the flattening of the natal cleft. Although skin flap techniques (Limberg, W- or Z-plasty) show relatively low recurrences rates (0-7%), they are traumatic, more complex, and are accompanied by higher rate of postoperative pain and wound complications [6,10,18,20]. Such operations are followed by substantial deforming scar formation and result in deterioration of the sacrococcygeal region’s normal anatomy, leading to poor aesthetic results.
An ideal surgical technique should provide a complete cure for IPD with a minimum risk of recurrence, be simple, require a short duration of hospitalization, give the lowest risk of complications, and guarantee a patient’s quick recovery. At the moment, the methods comprising asymmetric wound closure preceded by total excision of pilonidal tracts (Karydakis and Bascom’s techniques) mostly satisfy the requirements mentioned above, given the fact that more comparative controlled studies should be conducted for final conclusions. The postoperative results also depend on the age of the patient and the presence of comorbid diseases, which, as is well known, significantly affects the course of the wound healing process. This circumstance should be taken into account when investigating treatment results in comparative groups.
Intergluteal pilonidal disease is most prevalent among Caucasian males aged 18 to 48 years. This disease may drastically decrease the quality of life and lead to incapacity to work for up to several months. Considering the fact that persons in the 18-48 age group mainly comprise the employed social class, the identification of the most effective treatment method for IPD also gains social-economic importance.
In this study, our objective was to compare the Karydakis technique with wound marsupialization preceded by total excision of pilonidal tracts in the treatment of male patients with IPD regarding postoperative short-term complications, persistency of the postoperative pain, and duration of complete scar formation.
Methods
Patient selection: A total of 125 medical records of the patients treated for IPD during the period from January 2017 to December 2020 were extracted from the archive. The inclusion criteria were as follows: male patients aged 18-48 years who were referred to our clinic for both uncomplicated IPD (with only primary midline pores) and chronic complicated IPD (with secondary pilonidal orifices). The exclusion criteria were medical history of previous pilonidal surgeries, abscess presentations, and the presence of comorbidities.
A total of 60 patients either met the exclusion criteria or did not meet the inclusion criteria and were excluded from the study. The remaining included 65 patients were divided into 2 groups according to the IPD treatment technique: the marsupialization group (M-group, n = 33) and the Karydakis group (K-group, n = 32).
Surgical techniques: In all cases, surgery was performed under spinal anesthesia in the prone position. A dose of prophylactic cephalosporin was given intravenously in both groups during the induction of anesthesia. Methylene blue mixed with 10% hydrogen peroxide was injected into the sinus orifice(s) just before the incision. As pilonidal sinus excisions are performed by various senior surgeons in our team, the choice of the surgical technique was based on the surgeon’s preference and experience in the flap approach. Surgeons who proposed the marsupialization approach had previous experience with the procedure for at least 10 years and K-group – for at least 4 years.
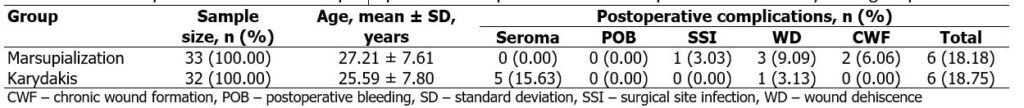
In the M-group, an oval excision was made, which covers the entire area where the sinus tracts extended. Hemostasis was accomplished by using electro¬cautery. After radically removing the sinus tracts, the skin edges were sutured to the sacral fascia at the midline from both sides of the wound utilizing 2/0 polypropyl¬ene Donati (vertical mattress) sutures, leaving open a narrow stripe along the wound in the midline (approximately 0.3 cm in width) as shown in Figure 1.
In the K-group, an asymmetrical elliptic excision was made with the lower and upper corners located approximately 1 cm lateral to the natal cleft; all defective tissues were removed until the healthy borders had been reached. The proximal edge of the wound was mobilized creating a tension-free skin flap. Afterward, the subcutaneous tissue was sutured to the sacral fascia creating a deviation towards the distal edge and lifting the natal cleft (absorbable suture material was utilized). And finally, the skin was closed with a Donati (vertical mattress) suture maintaining off-midline deviation of the suture line (using non-absorbable material). A suction drain was placed in the subcutaneous space, and was removed when drainage dropped below 10 mL/day. The two surgical techniques are illustrated in Figure 1.
Postoperative follow up: After the surgery, patients were examined, and the simple dressing was changed routinely every day. Sutures were removed in both groups 10-14 days after the surgery. Patients with delayed healing continued to be seen until complete healing was achieved. Patients were allowed to walk 2-3 days after surgery, and sitting was allowed only after healing of the wound and formation of the postoperative scar. Patients were then assessed weekly in the first month following discharge from the hospital and 3 months following the surgery. Postoperative depilation was performed in both groups.
Standard doses of nonsteroidal anti-inflammatory drugs (NSAIDs, particularly: Ketoprofen 100mg, Dexketoprofen 50mg, or Ketorolac 30mg) were used to manage the postoperative pain. Drugs were administered intravenously upon patients’ request based on subjective pain sensations in the postoperative wound area. None of the 65 cases required administration of opioid analgesics. As the analgesics were administered upon patients’ request and not routinely, we decided to use the total number of standard doses of NSAIDs utilized throughout the postoperative period as a criterion for evaluation of postoperative pain persistency. The retrospective design of our study, apparently, limited the usage of other pain evaluation scales such as visual analogue scale (VAS) or numeric rating scale (NRS).
Data related to the patients’ age, operation type, duration of complete wound healing (scar formation), postoperative complications (seroma formation, postoperative bleeding, surgical site infection, wound dehiscence, and chronic wound formation), and the total number of standard doses of NSAIDs were recorded in both groups. Recurrence rate was evaluated at 3 months post-surgery.
All obtained data were entered into a specially prepared chart.
Institutional review board (IRB) approval: The study was approved by the IRB of the Yerevan State Medical University (21-Oct-2021 N3-7/2021) stating that the study was in accordance with the Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects.
Informed consent: All 65 selected patients have given their consent to use the de-identified data from their medical records, the pre-, intra-, and postoperative photographs, and have signed an informed consent form developed according to the World Health Organization Ethics Review Committee (WHO ERC) requirements during the time period from January 2021 to February 2021.
Statistical analysis: Statistical analysis was performed using GraphPad Prism 8.0.1 and Microsoft Excel 2013 software. The mean and the standard deviation (SD) were measured for calculating numerical parameters, while the percentage was determined for categorical variables. In addition, Student’s independent sample T-test was used to compare the data. The results are presented as mean ± SD or proportion, as appropriate. A 2-tailed P-value of less than 0.05 was considered statistically significant.
Results
Treatment results of overall 65 patients were analyzed. All patients were male. The age difference between K (25.59 ± 7.80 years) and M (27.21 ± 7.61 years) groups was not statistically significant, p = 0.4005.
The mean duration of complete scar formation was 26.39 ± 11.14 days and 18.91 ± 7.48 days in the M- and K-groups, respectively. The difference was statistically significant: p = 0.0024 (CI = 95%, t = 3.171, df = 63). The Karydakis technique was found to be superior in terms of the duration of complete scar formation. The distribution, mean ± SD of the duration of complete scar formation in K- and M- groups is shown in Figure 2.
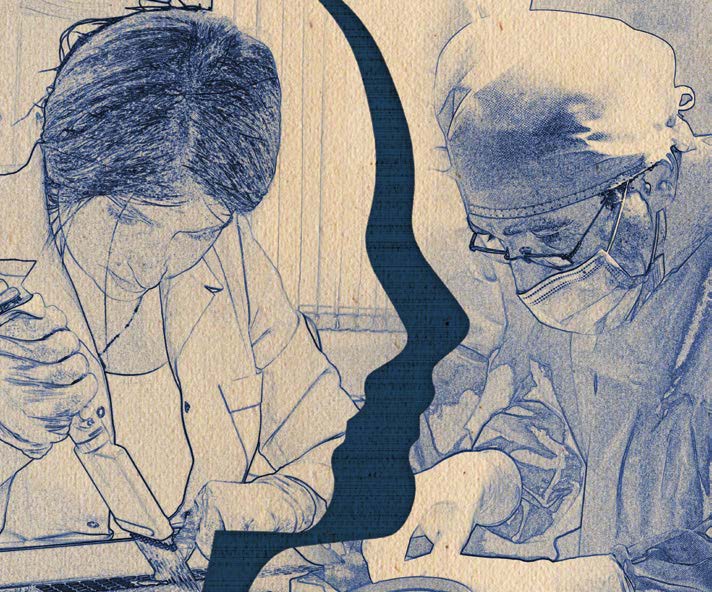
The rate of short-term complications in both groups was roughly the same: 6 cases (18.18%) in M-group and 6 cases (18.75%) in K-group. Seroma was the most prevalent type of complication: 5 cases in K-group and 0 in M-group. Wound dehiscence was the second most prevalent with 3 cases in M-group and 1 case in K-group. More detailed data on short-term postoperative complications in comparative groups are represented in Table 1.
Comparative analysis of the data related to the usage of NSAIDs showed that Karydakis surgery was associated with less persistency of postoperative pain: 5.84 ± 1.83 standard doses in K-group versus 9.15 ± 3.12 standard doses in M-group (p < 0.0001, CI = 95%, t = 5.186, df = 63). The cases with postoperative complications tended to require more analgesics than usual. Figure 3 represents the distribution, mean ± SD of the total number of standard doses of NSAIDs used per case.
All patients were followed up for 3 months postoperatively. The recurrence rates were 6.25% (n = 2) versus 15.15% (n = 5) in K- and M- groups, respectively; however, the results were considered statistically non-significant (p = 0.2539, CI = 95%, t = 1.151, df = 63).
Discussion
Karydakis technique was found to be superior over marsupialization in terms of the duration of complete scar formation, persistency of postoperative pain, and severity of short-term postoperative complications, and more research is needed to accurately measure recurrence rates. It is relatively easy to perform technically compared to other flap techniques, and the treatment results are comparable with the techniques mentioned above. Owing to the technical straightforwardness of the Karydakis procedure it can be easily adopted by practicing surgeons and requires minimal training.
The marsupialization technique can be mostly replaced by the Karydakis procedure in surgical practice, which will reduce the hospital stay days and, subsequently, the work-off period of the patients, as well as diminish the costs of hospitalization.
Although the Karydakis technique is superior in most notable aspects, in severely complicated cases with branched sinuses and multiple secondary orifices marsupialization technique still appears to be a better option.
Figure 4 represents a case of IPD with severely branched pilonidal sinuses and abscesses. Following the admission of the patient, the abscesses were drained through incisions under local anesthesia, and wounds were treated for 10 subsequent days with oral and topical antimicrobial agents and wound dressings. The patient underwent surgery on the eleventh day. Considering the severity of the disease, it was decided to use the marsupialization technique instead of the Karydakis. A butterfly-shaped asymmetrical incision was made in order to cover the whole affected area. The pilonidal tracts were removed en bloc at the healthy tissue borders. The horizontal incisions were closed with interrupted sutures; afterwards, the edges of the midline elliptic incision were sutured to the sacral fascia, leaving open a narrow stripe at the midline and a triangular area at the upper corner of the wound. The aforementioned areas eventually healed with secondary intention. The patient was discharged on the 41st day of the treatment and gained full working capacity after 20 additional days of rehabilitation period.
Limitations: The main limiting factors of our research were its retrospective design, relatively small sample sizes, and relatively short duration of follow up.
To reduce the risk of selection bias, the medical records of all 125 IPD patients treated at our clinic between January 2017 and December 2020 were extracted from the archive, after which the exclusion criteria were applied.
A surgeon selecting either of the two techniques usually has a biased intention (conscious or unconscious) to report the treatment outcomes favorably. However, in our clinic, the treatment results of the patients are ultimately assessed not by the attending doctor alone, but by a collegial examination. This assessment is more likely to be objective, hence reducing the risk of reporting bias.
The retrospective design also has limited the usage of more sophisticated tests, scales, or questionnaires in order to assess the postoperative pain level, ambulation and the ease of self-care, patient satisfaction, etc.
Relatively small sample sizes have limited us from accurately measuring postoperative morbidity and recurrence rates, as well as running statistic tests.
Hence, further research is needed to measure the abovementioned parameters more precisely.
Conclusions
Statistical analysis of the data from our research allows us to conclude that the Karydakis technique seems to be superior to the marsupialization technique in terms of the duration of complete wound healing (scar formation), as well as the recurrence rates in the treatment of male patients with IPD. Both techniques result in roughly the same rate of short-term postoperative complications, yet complications in the Karydakis technique are milder (seromas versus wound dehiscence and chronic wound formation). The pain sensations in the postoperative wound area are less persistent in the Karydakis procedure, hence it requires less postoperative analgesia.
Owing to a relatively faster recovery, choosing the Karydakis technique allows reducing the length of hospital stay, and, as a result, diminishes financial costs of the hospital (reduced maintenance costs, no excessive consumption of dressing materials, antiseptic solutions, and other drugs used in the course of the treatment).
Marsupialization technique is associated with a higher recurrence rate. However, the results were considered statistically non-significant and further research is encouraged to measure the recurrence rates more accurately.
Although the Karydakis technique is superior in most notable aspects, in severely complicated cases with branched sinuses and multiple secondary orifices, the marsupialization technique is still a better option because those cases require extensive excision and create large tissue defects.
Conflict of interests
The authors declare no competing interests.
Funding
Since the study was based solely on the analysis of data extracted from patients’ medical records, the process itself did not imply any expenses. Thus, the authors did not apply for financial support and declare that no funding from external sources.
Acknowledgments
We would like to acknowledge our entire surgical team for helping with the workflow and, of course, for performing the surgeries, the results of which we analyzed in our research, namely: H.V. Hovhannisyan, MD, G.S. Datumyan, MD, PhD, S.S. Shahbazyan, MD, PhD, M.S. Samsonyan, MD, and M.A. Sahakyan, MD.
References
- Akinci OF, Bozer M, Uzunköy A, Düzgün SA, Coşkun A. Incidence and aetiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg. 1999;165(4):339-42.
- Da Silva JH. Pilonidal cyst: cause and treatment. Dis Colon Rectum. 2000;43(8):1146-56.
- Doll D, Luedi MM, Evers T, Kauf P, Matevossian E. Recurrence-free survival, but not surgical therapy per se, determines 583 patients’ long-term satisfaction following primary pilonidal sinus surgery. Int J Colorectal Dis. 2015;30(5):605-11.
- Evers T, Doll D, Matevossian E et al. [Trends in incidence and long-term recurrence rate of pilonidal sinus disease and analysis of associated influencing factors] [Article in Chinese]. Zhonghua Wai Ke Za Zhi. 20111;49(9):799-803.
- Sarhan AE, Sherif T, Zakaria Y. A prospective randomized trial comparing modified Limberg flap and cleft lift procedure in the treatment of uncomplicated sacrococcygeal pilonidal disease. Egypt J Surg. 2016;35:89-95.
- Afşarlar CE, Yılmaz E, Karaman A et al. treatment of adolescent pilonidal disease with a new modification to the Limberg flap: Symmetrically rotated rhomboid excision and lateralization of the Limberg flap technique. J Pediatr Surg. 2013;48(8):1744-9.
- Khaira HS, Brown JH. Excision and primary suture of pilonidal sinus. Ann R Coll Surg Engl. 1995;77(4):242-4.
- McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008;336(7649):868-71.
- Søndenaa K, Andersen E, Nesvik I, Søreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10(1):39-42.
- Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002;45(11):1458-67.
- Chintapatla S, Safarani N, Kumar S, Haboubi N. Sacrococcygeal pilonidal sinus: historical review, pathological insight and surgical options. Tech Coloproctol. 2003;7(1):3-8.
- Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002;82(6):1169-85.
- Tokac M, Dumlu EG, Aydin MS, Yalcın A, Kilic M. Comparison of modified Limberg flap and Karydakis flap operations in pilonidal sinus surgery: prospective randomized study. Int Surg. 2015;100(5):870-7.
- Füzün M, Bakir H, Soylu M et al. Which technique for treatment of pilonidal sinus–open or closed? Dis Colon Rectum. 1994;37(11):1148-50.
- Sievert H, Evers T, Matevossian E et al. The influence of lifestyle (smoking and body mass index) on wound healing and long-term recurrence rate in 534 primary pilonidal sinus patients. Int J Colorectal Dis. 2013;28(11):1555-62.
- Solla JA, Rothenberger DA. Chronic pilonidal disease. An assessment of 150 cases. Dis Colon Rectum. 1990;33(9):758-61.
- Khanna A, Rombeau JL. Pilonidal disease. Clin Colon Rectal Surg. 2011;24(1):46-53.
- Spivak H, Brooks VL, Nussbaum M, Friedman I. Treatment of chronic pilonidal disease. Dis Colon Rectum. 1996;39(10):1136-9.
- Søndenaa K, Nesvik I, Andersen E, Søreide JA. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomised trial. Eur J Surg. 1996;162(3):237-40.
- Karaca T, Yoldaş O, Bilgin BÇ, Ozer S, Yoldaş S, Karaca NG. Comparison of short‑term results of modified Karydakis flap and modified Limberg flap for pilonidal sinus surgery. Int J Surg. 2012;10(10):601-6.
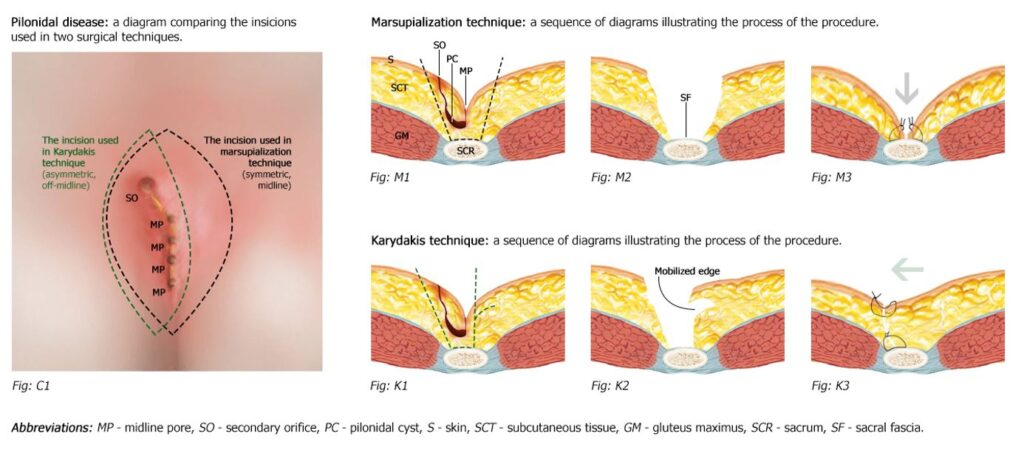
Figure 1: Comparative illustrations of marsupialization and Karydakis techniques.
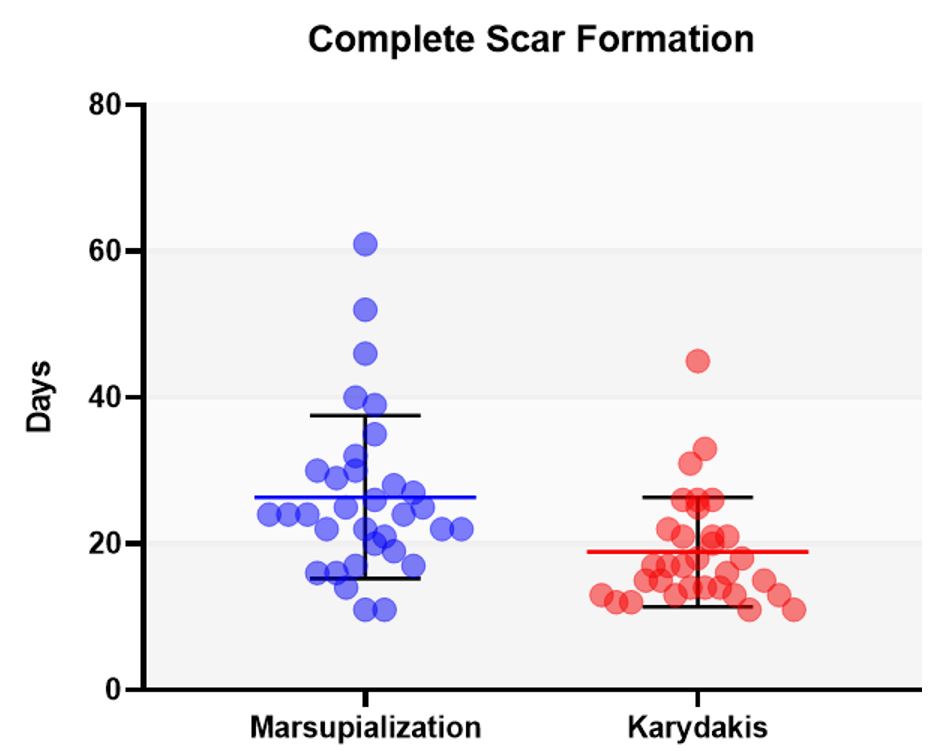
Figure 2: Comparative diagram representing the distribution of the mean (± SD) duration of complete scar formation in both techniques.
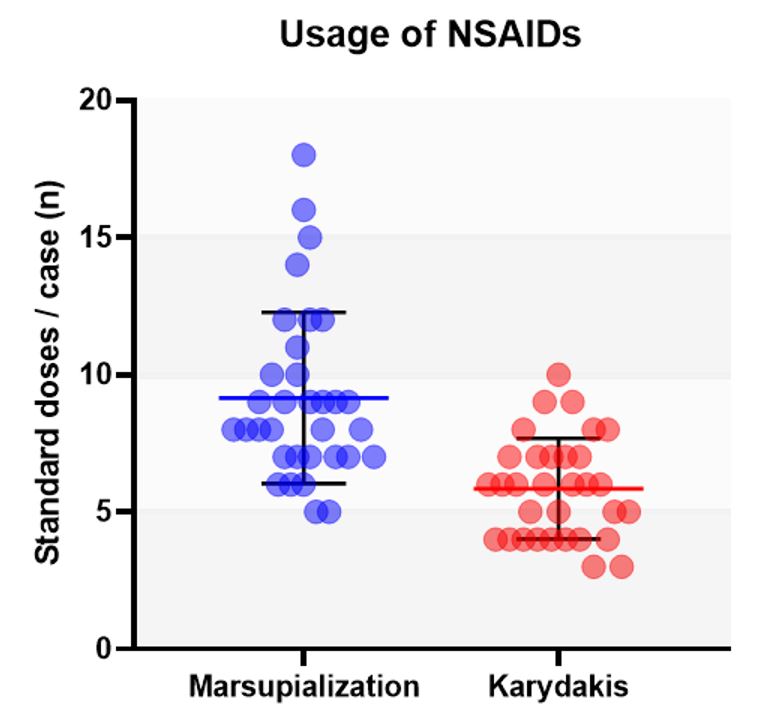
Figure 3: Comparative diagram representing the distribution of the mean (± SD) total number of standard doses of NSAIDs used per case.
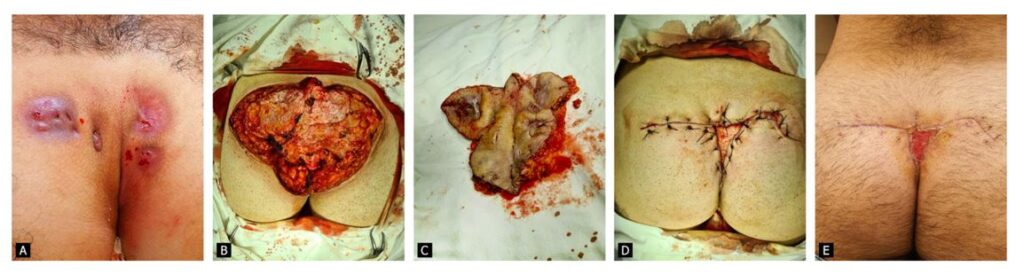
Figure 4: Branched intergluteal pilonidal disease. A. Preoperative photograph prior to incision and drainage. B. Intraoperative photograph after excision of the affected areas. C. Intraoperative photograph of the excised tissue. D. Intraoperative photograph after closing the tissue defect. E. Postoperative photograph 19 days after surgery.
Table 1: The comparison of short-term postoperative complications in Marsupialization and Karydakis groups