INTRODUCTION
COVID-19 outbreak has brought new challenges in different areas of medicine, including mental health. Its global impact will become evident much later, but we are already observing a total increase in population anxiety and concern about health issues. People are more afraid for their health and life. And while the global health burden due to COVID-19 mortality is reported to be overestimated [1], this effect cannot be ignored.
One of the most vulnerable patient groups is those with obsessive-compulsive disorder (OCD). The fear of contamination and obsessive thoughts about the correctness of actions are common symptoms of this disorder, and it is logical to assume that these symptoms will intensify under current conditions.
Diagnostic and Statistical Manual for Mental Disorders (DSM-5) defines OCD as a disorder containing obsessions – repetitive and intrusive thoughts that cause distress, and compulsions – behavioral responses aimed to reduce this distress [2]. The disorder is fairly heterogeneous, but the fear of contamination is one of the most common symptoms [3]. In its turn, the general fear of contamination can be divided into two main types: the contact one and the mental one. The contact contamination fear is based on avoiding and cleaning the actions justified by the fear to be infected, and has a rational core, although it is usually exaggerated or overestimated. The so-called mental contamination[4], or the feeling of the incompleteness (INC) or not-just right experiences (NJRE) [5,6] is based on a feeling of disgust or internalized disturbance, without clear fear of the dangerous outcome.
In particular, we noticed an increase in the num ber of patients with OCD requesting psychiatric help in Armenia. However, along with the expected exacerbation of symptoms, we also observed some positive influence of the quarantine on OCD patients in Armenia. Generally, it can be described as differentiation and rationalization of the contamination obsessions in OCD patients.
The aim of the study was to observe the impact of the COVID-19 pandemic on patients with contamination fear and how it can be used to improve psychotherapeutic treatment.
MATERIALS AND METHODS
Following the COVID-19 outbreak in Armenia between April 2020 and March 2021, we observed 57 patients with OCD with the prevalence of contamination fear who experienced both contact and mental contamination obsessions. Of these 57 patients, 33 met inclusion criteria (see below) and were involved in our study.
We assessed the condition of patients at the beginning and after 3 and 6 months of therapy using Yale-Brown Obsessive-Compulsive Scale (Y-BOCS)
– a questionnaire that includes 10 questions about obsessions and compulsions, evaluated from 0 to
- Total Y-BOCS score assesses the severity of the condition: 0-7 pts – no OCD or subclinical condition, 8-15 – mild OCD, 16-23 0 moderate OCD, 2431 – Severe OCD, 32-40 – extremely severe OCD. Y-BOCS is considered an optimal evidence-based and accurate assessment instrument for OCD [7]. The scale was translated forward to Armenian and back by specialized translators and currently is in the process of
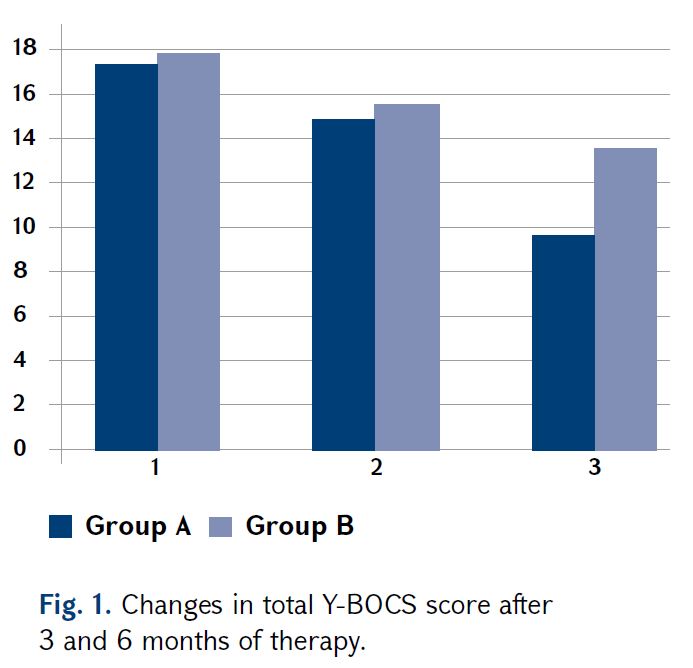
The patients were divided into 2 groups, comparable by age, gender and condition severity. Group A (n = 17) included 8 men and 9 women with an average age of 29.4 years and an average Y-BOCS score of 17.35 at the start of the study. Group B (n = 16) included 6 men and 10 women with an average age of 29 years and an average Y-BOCS score of 17.81 at the start of the study.
Both groups have been treated using permanent exposure therapy and mild doses of antidepressants – clomipramine 50-75 mg/daily or paroxetine 10-20 mg daily. In addition, in group A we involved an active educational block about anti-infective measures. It included a detailed and reasonable description of anti-infective measures, accompanied with additional exposure sessions with the practice of correct anti-coronavirus measures, such as wearing and removing masks and gloves, maintaining social distance and washing hands. In group B, instead of this standard protocol, we offered instead cognitive-behavioral therapy for OCD. Inclusion criteria: OCD meeting ICD-10 criteria, the prevalence of contamination fear in the clinical picture of the disorder, permanent cognitive-behavioral therapy for 6-month period, absence of comorbid disorders.
Exclusion criteria: age under 16, upper-mild doses of pharmacotherapy with antidepressants, use of other medication in treatment.
All participants signed informed consent about including in the study and were informed that any data will be presented anonymously.
Statistical analysis was performed using Microsoft Excel and SPSS Statistics 24.
RESULTS
In both groups, positive changes were observed after 6 months of combined treatment. However, we observed a significant difference between total average treatment efficacy evaluation between groups A and B (Fig. 1). In group A, the average total Y-BOCS score decreased from 17.35 to 9.65 (p<0.05), while in group B – from 17.81 to 13.5 (p<0.05). The difference was statistically significant: 44.4% versus 24.2% (p<0.05), which indicated the effectiveness of additional approaches used in group A in improving the general condition of patients.
Specific types and subtypes of symptoms were assessed using Y-BOCS Symptom Checklist. In particular, we evaluated the key symptoms connected to contamination: Concerns or disgust with bodily waste or secretions (e.g., urine, feces, saliva); Concern with dirt or germs; Excessive concern with environmental contaminants (e.g. asbestos, radiation, toxic waste); Excessive concern with household items (e.g., cleansers, solvents); Excessive concern with animals (e.g., insects); Bothered by sticky substances or residues; Concerned will get ill because of contaminant; Concerned will get others ill by spreading contaminant (Aggressive), as well as according to compulsions: excessive or ritualized handwashing; Excessive or ritualized showering, bathing, tooth brushing, grooming, or toilet routine involves cleaning of household items or other inanimate objects; Other measures to prevent or remove contact with contaminants.
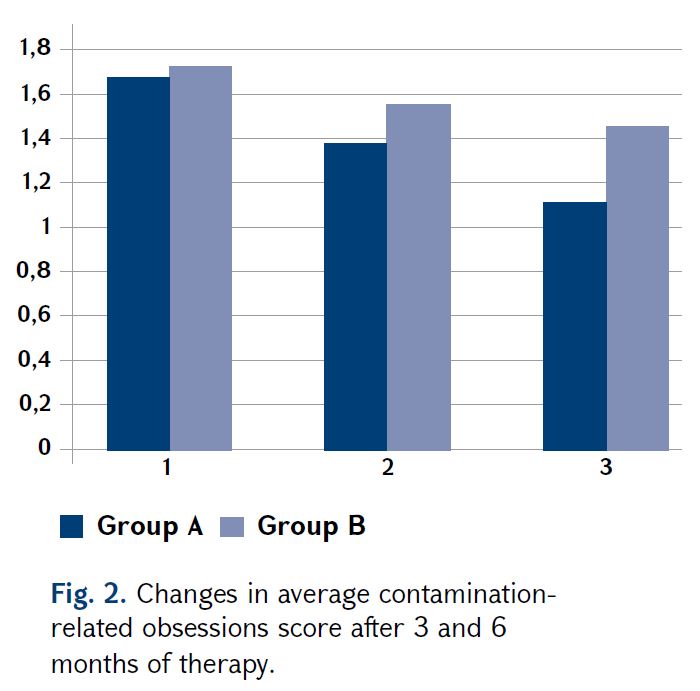
As a result of treatment, we observed a decrease in both obsessive and compulsive symptoms. In the case of obsessions, we saw the same picture as in general Y-BOCS score. Treatment efficacy was significantly higher in Group A – from 1.67 to 1.12, compared with Group B – from 1.71 to 1.45 (p<0.05) (Fig. 2).
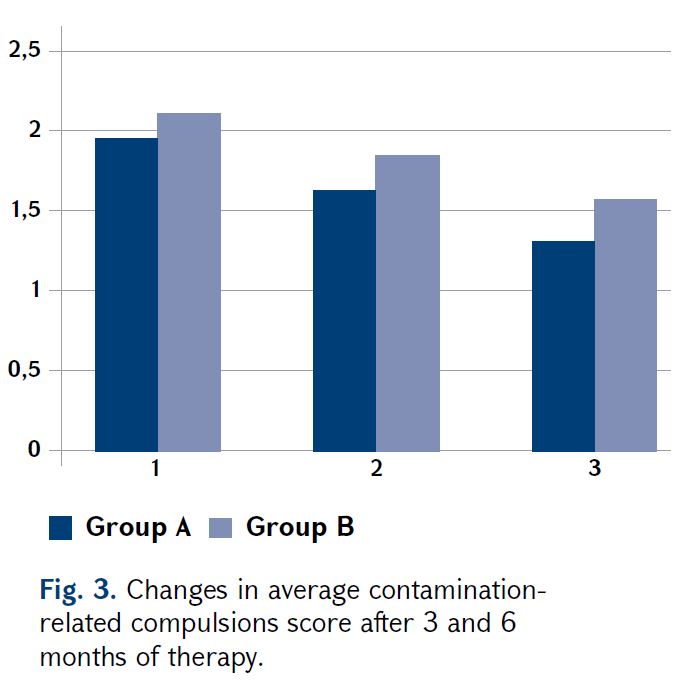
In contrast, there was no significant difference in the improvement of compulsory actions between the two groups. The positive changes that we observed in both groups were approximately similar: Group A – from 1.96 to 1.31, or 33.2%, Group B
– from 2.12 to 1.51, or 28.8% (Fig. 3).
Notably, the biggest difference in treatment efficacy between groups was observed for the three symptoms most associated with mental contamination: concerns or disgust with bodily waste or secretions – 34.1% improvement in Group A versus 6.1% in group B; being bothered by sticky substances or residues – 43% versus 8.9%; concerned will get ill because of contaminant – 35.6% versus 13%. This suggests that the therapeutic approach of group A is especially effective in treating the symptoms of mental contamination.
DISCUSSION
As it was mentioned above, contamination obsessions consist of two main subtypes – contact contamination and mental contamination. These two types are interrelated and can appear both separately or together [8]. Moreover, many researchers suppose mental contaminations and their components, such as INC or NJRE, are not only connected to obsessive fear of contamination, but also have a regulatory function for compulsions (e.g. hand washing) [9-11].
Compared to the mental ones, the contact contaminations are treated more effectively during the Exposure and Response Prevention Therapy [8], which is considered the standard treatment for OCD [3,6,12]. The explanation is that these obsessions are more reasonable and trigger clearer and more consistent actions, which can adapt to a given situation. There are also data about the patients with a prevalence of INC/NJREs, who show poorer treatment response and significantly higher drop out levels during exposure with response prevention therapy (ERP) [13,14].
As our study showed, a novel approach based on adding features related to the COVID-19 anti-infective measures – both theoretical and practical – gave a significant advantage in reducing INC/NJRE symptoms (32.9% vs. 15.2%, p<0.05) and lead to better average improvement of Y-BOCS score (44.4% vs. 24.2%, p<0.05). Only 2 of 17 patients in Group A showed no significant improvement after 6 months of therapy, while in Group B, the state of 5 out of 16 patients remained almost unchanged at the end of the study.
Further pathopsychological analysis showed three different ways of reducing the significance of INC and NJRE.
The first was observed in patients with obsessions of control and was connected to the development of detailed, even “ritualized” precautionary actions – wearing a protective mask and gloves, disinfecting hands, clothing and surfaces, maintaining social distance, etc. As they report, compliance with all the necessary measures brings a sense of satisfaction compared to performing pathological rituals and reduces INC and NJRE approximately equally. This leads to a decrease in compulsions and brings a higher level of feeling of fullness and correctness. The second way was also connected with precautionary actions, but mostly affected INC, which is known to act as a trigger of compulsions [3]. The clinical difference between these patients was that this group had a clearer understanding and distinction in their feelings. In this case, the patients showed a reduction of compulsory actions but the feeling of internalized discomfort retained. So, despite the fact that they had spent less time and energy on rituals, subjective assessment of their condition had changed slightly. Although we did not see a special effect on the NJRE, we did receive a significant improvement in the intensity of compulsions against the background of mental contamination fear, outweighing such changes during the therapy under usual conditions.
The third way was characterized by a prior increase in the fear of contact contamination. These patients appeared in severe or even extreme conditions, expressed in excessive anxiety and panic. Accordingly, their mental contamination feelings receded into the background, becoming less important. We emphasized this phenomenon during the stage of rationalization of contact obsessions. All patients almost similarly noticed that they realized the meaninglessness and unimportance of those feelings after experiencing reality-based severe anxiety about the serious risk for their health. After several ERP sessions, we gained a reduction of contact contamination obsessions levels without returning to the previous levels of mental obsessions.
Thereby, in the initial 3-4 sessions, we had a temporary increase in symptoms that were more controllable, and a decrease in symptoms that were treated worse. In the case of successful treatment of contact contamination obsessions, none of the patients returned to their previous levels of mental obsessions during the period of 2-6 weeks.
CONCLUSION
Given the small sample sizes and short follow-up periods, we remain cautious in our conclusions. Nevertheless, we want to draw attention to the fact that the presence of a real threat of infection in many patients leads to a rethinking of their symptoms, reassessment of their relative importance and helps to achieve better results in therapy.
Our most important finding is that addition of reality-based and emotionally significant features of contamination control and prevention may dramatically improve treatment outcomes for mental contamination obsessions.
It should also be noted that the period of pandemics, as well as the post-pandemic period, can be used for further intensive research in this area in a larger cohort of patients. In particular, there is a need for professional evaluation of the condition of patients using specific scales, adding Dimensional Obsessive-Compulsive Scale (DOCS), Obsessive-Compulsive Trait Core Dimensions Questionnaire (OCTCDQ), Disgust Propensity and Sensitivity Scale-revised (DPSS-R), Depression, Anxiety, and Stress Scale-21 (DASS-21) for a more detailed evaluation of OCD symptoms and understanding the role of comorbid conditions. Another main point is monitoring the stability and the duration of the positive effect, which must be assessed at least twice after 6 and 12 months. It must also be assessed after enough time has passed during quarantine, and after a while the infection factor has lost its relevance.
In the background of the COVID-19 outbreak, we expect an increase in the number of new cases of OCD, as well as increased frequency of exacerbations in those who already have OCD. Thus, it seems very important to notice and develop all the opportunities that can help to achieve better results in treatment.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). Arlington, VA. American Psychiatric Publishing. 2013.
- Belloch A., Fornés G., Carrasco A., López-Solá C., Alonso P., Menchón J.M. Incompleteness and not just right experiences in the explanation of Obsessive-Compulsive Disorder. Psychiatry Res. 2016;236:1-8.
- Coles M.E., Frost R.O., Heimberg R.G., Rhéaume J. “Not just right experiences”: perfectionism, obsessive- compulsive features and general psychopathology. Behav Res Ther. 2003;41(6):681-700.
- Coles M.E., Ravid A. Clinical presentation of not- just right experiences (NJREs) in individuals with OCD: Characteristics and response to treatment. Behav Res Ther. 2016;87:182-187.
- Cougle J.R., Fitch K.E., Jacobson S., Lee H.J. A multi- method examination of the role of incompleteness in compulsive checking. J Anxiety Disord. 2013;27(2):231-239.
- Foa E.B., Abramowitz J.S., Franklin M.E., Kozak M.J. Feared consequences, fixity of belief, and treatment outcome in patients with obsessive-compulsive disorder. Behavior Therapy. 1999;30(4):717-724.
- Foa E.B., Yadin E., Lichner T.K. Exposure and response (ritual) prevention for obsessive-compulsive disorder: Therapist guide (2nd ed.). Exposure and Response (Ritual) Prevention for Obsessive-Compulsive Disorder: Therapist Guide (2nd ed.). 2018.
- Mathes B.M., Kennedy G.A., Wilver N.L., Carlton C.N., Cougle J.R. A multi-method analysis of incompleteness in behavioral treatment of contamination-based OCD. Behav Res Ther. 2019;114:1-6.
- Melli G., Bulli F., Carraresi C., Tarantino F., Gelli S., Poli A. The differential relationship between mental contamination and the core dimensions of contact contamination fear. J Anxiety Disord. 2017;45:9-16.
- Rapp A.M., Bergman R.L., Piacentini J., McGuire
J.F. Evidence-based assessment of obsessive-compulsive disorder. J Cent Nerv Syst Dis. 2016;8:13-29.
- Roussel Y., Giraud-Gatineau A., Jimeno M.T. et al. SARS-CoV-2: fear versus data. Int J Antimicrob Agents. 2020;55(5):105947.
- Summerfeldt L.J. Understanding and treating incompleteness in obsessive-compulsive disorder. J Clin Psychol. 2004;60(11):1155-1168.
- Summers B.J., Fitch K.E., Cougle J.R. Visual, tactile, and auditory “not just right” experiences: associations with obsessive-compulsive symptoms and perfectionism. Behav Ther. 2014;45(5):678-689.
- Wahl K., Salkovskis P.M., Cotter I. ‘I wash until it feels right’ the phenomenology of stopping criteria in obsessive- compulsive washing. J Anxiety Disord. 2008;22(2):143-161.